
S296
24th European Congress of Psychiatry / European Psychiatry 33S (2016) S116–S348
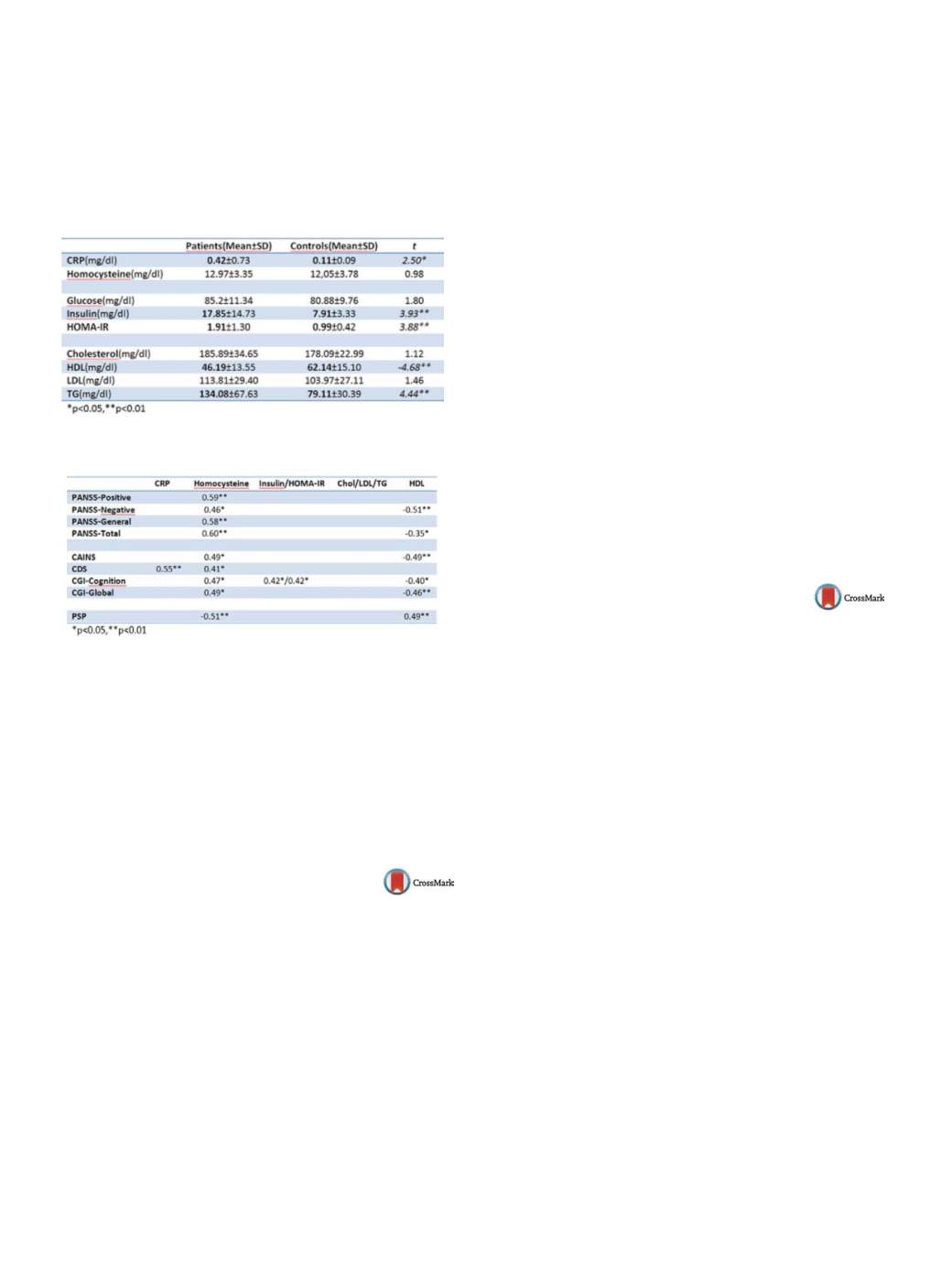
Conclusions
1. CRP, a potential inflammatory biomarker in
schizophrenia, is related to depression severity. Homocysteine,
representing an oxidative stress, is related to positive, negative,
cognitive and depressive symptoms severity, and worse function-
ing. 2. Patients with schizophrenia have lower HDL–related to neg-
ative and cognitive symptoms severity and worse functioning–and
insulin resistance – related to worse cognition –.
Table 1
Table 2
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
References
[1] Kirkpatrick B, Miller B, García-Rizo C, Fernandez-Egea E.
Schizophrenia: a systemic disorder. Clin Schizophr Relat Psy-
choses 2014;8(2):73–9.
[2] Miller BJ, Buckley P, et al. Meta-analysis of cytokine alterations
in schizophrenia: clinical status and antipsychotic effects. Biol
Psychiatry 2011;70(7).
http://dx.doi.org/10.1016/j.eurpsy.2016.01.635EW518
Clinical and functional response to
paliperidone palmitate in early
schizophrenia–A retrospective
observational study in newly
diagnosed patients treated over a
12-month period
L. Hargarte
r 1 ,∗
, P . Bergmans
2 , P. Cherubin
3 , A.Schreiner
11
Janssen Cilag Germany, Medical Affairs EMEA, Neuss, Germany
2
Janssen Cilag Netherlands, Biostatistics, Tilburg, Netherlands
3
Janssen Cilag France, Medical Affairs EMEA, Issy-Lès-Moulineaux,
France
∗
Corresponding author.
Introduction
Data on clinical outcomes with long-acting antipsy-
chotic treatment in young, newly diagnosed patients with
schizophrenia is sparse.
Objectives
To explore hospitalization, drug utilization and
clinical outcomes from medical records of newly diagnosed
schizophrenia patients during first 12 months of treatment with
once-monthly paliperidone palmitate (PP).
Methods
International, multicenter, retrospective, observational
study. Outcomes presented: baseline (BL) characteristics and
demographics, clinically relevant improvements in disease sever-
ity (ie
≥
20% decrease in PANSS or BPRS total score or CGI-S
Change
≥−
2 or CGI-C
≥
3, with no score showing worsening) and
clinically relevant functional improvement (i.e. change in PSP total
score
≥
+7 points or change in GAF total score
≥
+20 points, with
no score showing worsening) from BL to last-observation-carried-
forward endpoint (LOCF-EP) within 12-month documentation
period, mean mode PP dose and adverse drug reactions.
Results
Eighty-four patients analyzed: 69% male, mean age at
initiation of PP was 24.1 (SD2.7) years, mean BL weight was 78.7
(SD16.0) kg and 80.0 (SD14.7) kg at LOCF-EP, with a mean change
of 1.2 (SD3.9) kg; mean time from first psychotic episode to initi-
ation of PP was 5.5 (SD3.3) months. At LOCF-EP 86.6% achieved a
clinically relevant improvement (71/84, Kaplan-Meiermedian time
from initiation of PP: 52.4 days). 63.4% achieved a clinically relevant
functional improvement (52/84, Kaplan-Meier median time from
initiation of PP: 53.1 days). PP mean mode maintenance dose was
96.4 (SD19.8) mg. ADRs reported in
≥
5% of patients were weight
increase 9.1% and hyperprolactinemia 5.7%.
Conclusions
Treatment with once-monthly PP was well tolerated
and associated with clinically relevant improvements in disease
severity and functioning in young, newly diagnosed schizophrenia
patients.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.636EW519
Early schizophrenia patients treated
with once-monthly paliperidone
palmitate over a 12-month period - a
retrospective observational study
L. Hargarter
1 ,∗
, P . Bergmans
2 , P. Cherubin
3 , A. Schreiner
11
Janssen Cilag Germany, Medical Affairs EMEA, Neuss, Germany
2
Janssen Cilag Netherlands, Biostatistics, Tilburg, Netherlands
3
Janssen Cilag France, Medical Affairs EMEA, Issy-Lès-Moulineaux,
France
∗
Corresponding author.
Introduction
Little is known about patient characteristics and
rehospitalization in newly diagnosed patients with schizophrenia
treated with long-acting antipsychotics.
Objectives
To retrospectively explore hospitalizations, drug uti-
lization and clinical outcomes from medical records of young,
newly diagnosed schizophrenia patients during the first 12
months of treatment with once-monthly paliperidone palmitate
(PP).
Methods
International, multicenter, retrospective, observational
study. Outcomes presented are patient characteristics, reason for
PP initiation and hospitalization data.
Results
Eighty-four patients were analyzed: mean age (years)
at first psychotic episode was 23.8 (SD2.6), 23.9 (SD2.6) at first
antipsychotic treatment and 24.1 (SD2.7, range 19-29) at PP initia-
tion. Time between first antipsychotic treatment and PP initiation
was 4.8 (SD: 3.4, range: 0-12) months. At PP initiation, 42.9% of
patients were in hospital, primarily for the management of the first
episode/relapse (97.2%). Reason for PP initiation was: LAT favored
over oral treatment for relapse prevention (56%), partial/non adher-
ence with previous oral medication (20.0%), convenience (15.5%)
or limited access to health care systems (2.4%). Mean time (days)
between admission and initiation of PP, and between initiation
of PP and discharge from hospital was 28.8 (SD23.0) and 23.2
(SD24.5), respectively. 96.4% of patients were not hospitalized dur-
ing the 12-month PP treatment period. 3/84 patients (3.6%) had
a single hospitalization of 15.7 (SD: 8.1) days for management of
episode/relapse.


















