
S298
24th European Congress of Psychiatry / European Psychiatry 33S (2016) S116–S348
percent of patients clinically improved on AM. Blood parameters
were in the normal range.
Discussion
Within the limitations of themethodology, our results
show a reduction in psychiatric bed use in the year following AM
initiation on an intention to treat basis. The reduction in bed use
equates to a minimum annual saving of
£
14,250 per patient. AM at
the median study dose costs
£
2645 per year.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.640EW523
Coping strategies and quality of life in
schizophrenia outpatients treated by
Psychopharmacs - cross-sectional
study
M. Holubova
1 , 2 ,∗
, J. Prasko
1, R. Hruby
3, D. Kamaradova
1,
M. Ociskova
1, K. Latalova
1, A. Grambal
11
Faculty of medicine and dentistry- Palacky university Olomouc-
university hospital Olomouc, department of psychiatry, Olomouc,
Czech Republic
2
Regional hospital Liberec, department of psychiatry, Liberec, Czech
Republic
3
Psychiatric outpatient department, Martin, Slovakia
∗
Corresponding author.
Introduction
Themodern psychiatric viewof schizophrenia spec-
trum disorders and their treatment has led to an increasing focus
on coping strategies and quality of life of these patients.
Objectives
Understanding the relationship between quality of life
and coping strategies can help in finding those coping strategies
that enhance the quality of life. It is important to study the inner
experience and striving of patients because of connection with
well-being and treatment adherence.
Aims
: In the present study, the authors examined the relation-
ship between demographic data, the severity of symptoms, coping
strategies, and quality of life in psychotic outpatients.
Methods
Psychiatric outpatients who met ICD-10 criteria for
a psychotic disorder (schizophrenia, schizoaffective disorder, or
delusional disorder) were recruited in the study. Questionnaires
measuring the coping strategies (SVF-78), the quality of life (Q-
LES-Q), and symptoms severity (objective and subjective clinical
global impression–objCGI; subjCGI) were assessed. Data were ana-
lysed using one-way ANOVA, Mann-Whitney U-test, Pearson and
Spearman correlation coefficients, and multiple regression analy-
sis.
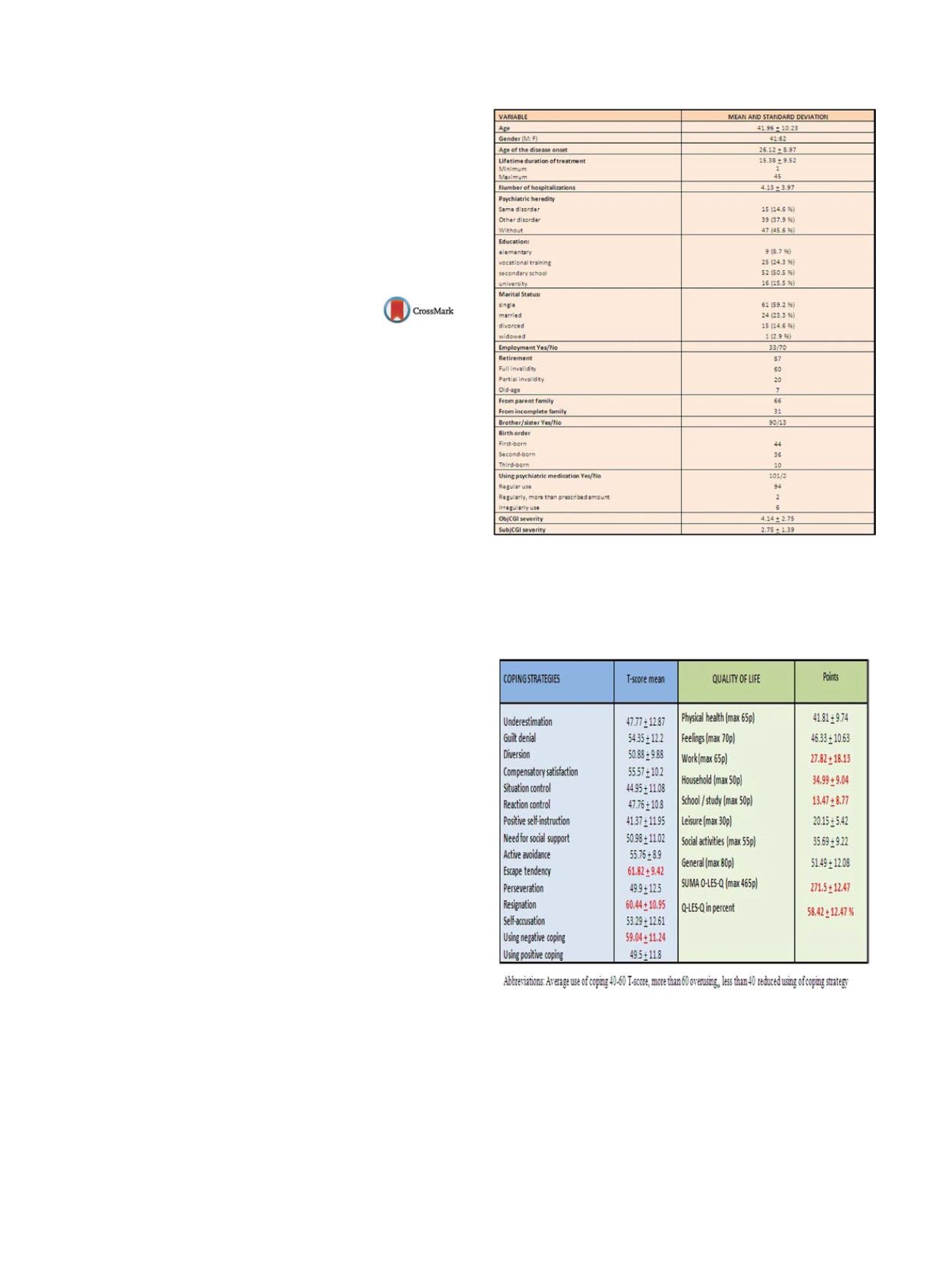
Results
One hundred and nine psychotic outpatients were
included in the study. The QoL was significantly related to the
Positive and Negative coping strategies. The severity of disorder
highly negatively correlated with the QoL score. Stepwise regres-
sion analysis showed that symptoms severity (subjCGI), Positive
coping strategies (especially Positive Self-instruction), Difference
between the objCGI and subjCGI and Negative coping strategies
explain totally 53.8% of variance of the QoL (Tables 1–3).
Conclusions
Our study suggests the importance of utilizing the
Positive coping strategies in improving the quality of life in patients
with psychotic disorders.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
Table 1
Description of the sample, demographic and clinical data.
Table 2
Description of using coping strategies and quality of life in
schizophrenic outpatients.
Average use of coping 40-60 T-score, more than 60 overusing,
less than 40 reduced use of coping strategy.


















