
24th European Congress of Psychiatry / European Psychiatry 33S (2016) S116–S348
S301
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.644EW527
Quality of care for medical
comorbidities among patients with
and without schizophrenia
M. Jørgensen
1 ,∗
, J. Mainz
1 , S. Paaske Johnsen
21
Aalborg university hospital, psychiatry, Aalborg, Denmark
2
Aarhus university hospital, department of clinical epidemiology,
Aarhus N, Denmark
∗
Corresponding author.
Introduction
The association between schizophrenia and quality
of care for medical comorbidities in universal health care systems
remains unclear.
Objectives
To elucidate whether equal access also implies equiv-
alent and sufficient care.
Aims
To compare the quality of care for heart failure, diabetes
and chronic obstructive pulmonary disease (COPD) among patients
with and without schizophrenia in Denmark.
Methods
In a nationwide population-based cohort study, we
used Danish national registries to estimate the risk of receiving
guideline recommendeddisease-specific processes of care between
2004 and 2013.
Results
Compared to patients without schizophrenia, patients
with schizophrenia had lower chance of receiving high overall qual-
ity of care (
≥
80% of recommended processes of care) for heart
failure (Relative risk [RR] 0.67, 95% CI: 0.48-0.92), diabetes (RR 0.84,
95% CI: 0.79-0.89) and COPD (RR 0.82, 95% CI: 0.72-0.93) as well
as lower chance of receiving individual disease-specific processes
of care including treatment with beta-blockers (RR 0.87, 95% CI:
0.79-0.96) in heart failure care and measurement for albuminuria
(RR 0.96, 95% CI: 0.93-0.99), eye examination at least every second
year (RR 0.97, 95% CI: 0.94-0.99) and feet examination (RR 0.96, 95%
CI: 0.93-0.99) in diabetes care. Diabetic patients with schizophre-
nia also had lower chance of receiving antihypertensive (RR 0.84,
95% CI: 0.73-0.96) and ACE/ATII inhibitors (RR 0.72, 95% CI: 0.55-
0.94). In COPD care, patients with schizophrenia had lower chance
of receiving LAMA/LABA medication (RR 0.92, 95% CI: 0.87-0.98),
however, higher chance of treatment with non-invasive inhalation
(RR 1.85, 95% CI: 1.61-2.12).
Conclusions
Quality of care for three medical comorbidities was
suboptimal for patients with schizophrenia.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.645EW528
Efficacy and tolerability of switching
to long-acting injectable (LAI)
aripiprazole in outpatients with
schizophrenia
B. Fernández-Abascal Puente , M. Juncal Ruiz
∗
,R. Landera Rodríguez
Hospital Universitario Marqués de Valdecilla, Psychiatry, Santander,
Spain
∗
Corresponding author.
Introduction
Switching antipsychotics is a therapeutic alterna-
tive for managing side-effects, or efficacy and compliance issues.
Aim
To evaluate the efficacy and tolerability of switching to LAI-
aripiprazole in patients who had insufficient response or were
intolerant to the previous antipsychotic, or required a more con-
venient treatment regimen.
Methods
This was a prospective, observational, 6-months study
carried out in 45 outpatients with schizophrenia who were
clinically stabilized but a switching to another antipsychotic
was clinically indicated. Patients who required hospitaliza-
tion, treatment discontinuation or adding another antipsychotic
(including supplementation with oral-aripiprazole) were consid-
ered treatment failures. Switching was considered successful if
the side-effect/symptom/adherence/convenience improved or, if
applicable, disappeared.
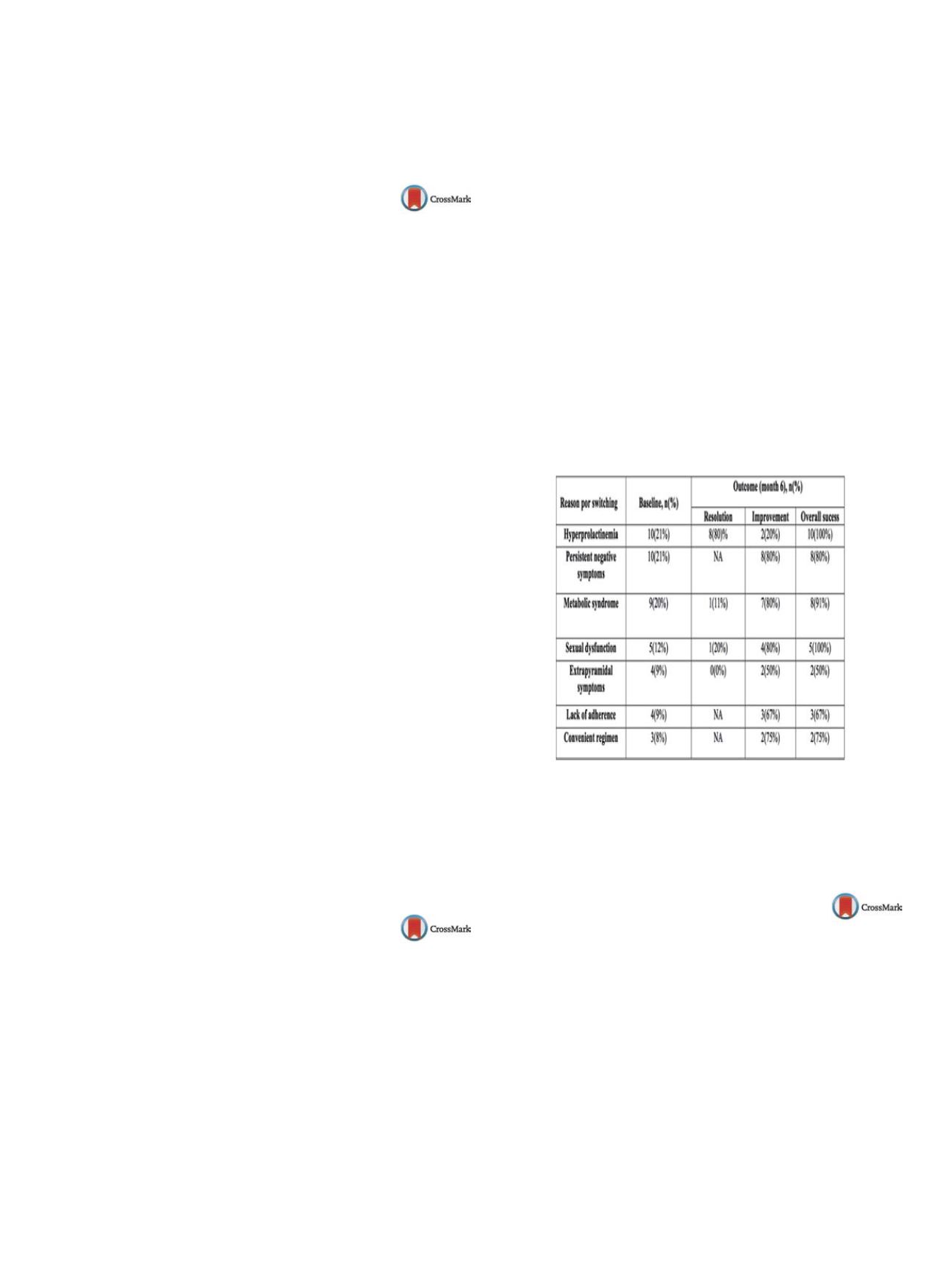
Results
Patients aged 38 years, 51% women, and previ-
ous antipsychotics comprised: LAI-paliperidone (42%), oral-
aripiprazole (22%), oral-olanzapine (11%), oral-risperidone (7%),
LAI-risperidone (4%) and others (14%). The efficacy results of
the switching are presented in the table. Of the 45 patients,
7 (15%) were considered treatment failures: 3 patients were
hospitalized due to recurrence of psychotic symptoms, 2 dis-
continued LAI-aripiprazole, and 2 required supplementation with
oral-aripiprazole
( Table 1 ).Conclusions
Our results suggest that switching to LAI-
aripiprazole is an efficacious strategy for managing some
antipsychotic-induced side-effects, persistence of negative
symptoms and/or lack of treatment adherence.
Table 1
.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.646EW529
Visual memory deficits and symptoms
in schizophrenia
D. Kontis
1 , 2 ,∗
, E. Theochari
1 , 2, V. Grigoriou
1, K. Goulas
1,
M. Kafritsa
1, D. Vassos
1, A. Andreopoulou
1, S. Vassilouli
1,
D. Giannakopoulou
1, E. Tsaltas
21
Psychiatric Hospital of Attica, Unit for the Study of Cognition in
Psychosis, Athens, Greece
2
Athens University Medical School, 1st Department of Psychiatry,
Athens, Greece
∗
Corresponding author.
Introduction
Cognitive deficits have been associated with nega-
tive, but not positive, symptoms in schizophrenia.
Aim
The investigation of the relationship of visual memory per-
formance with schizophrenia symptoms.
Patients and methods
Forty individuals with schizophrenia who
were referred to our Unit were assessed using the Benton
Visual Retention Test (BVRT) (visual memory), the Positive and


















