
S300
24th European Congress of Psychiatry / European Psychiatry 33S (2016) S116–S348
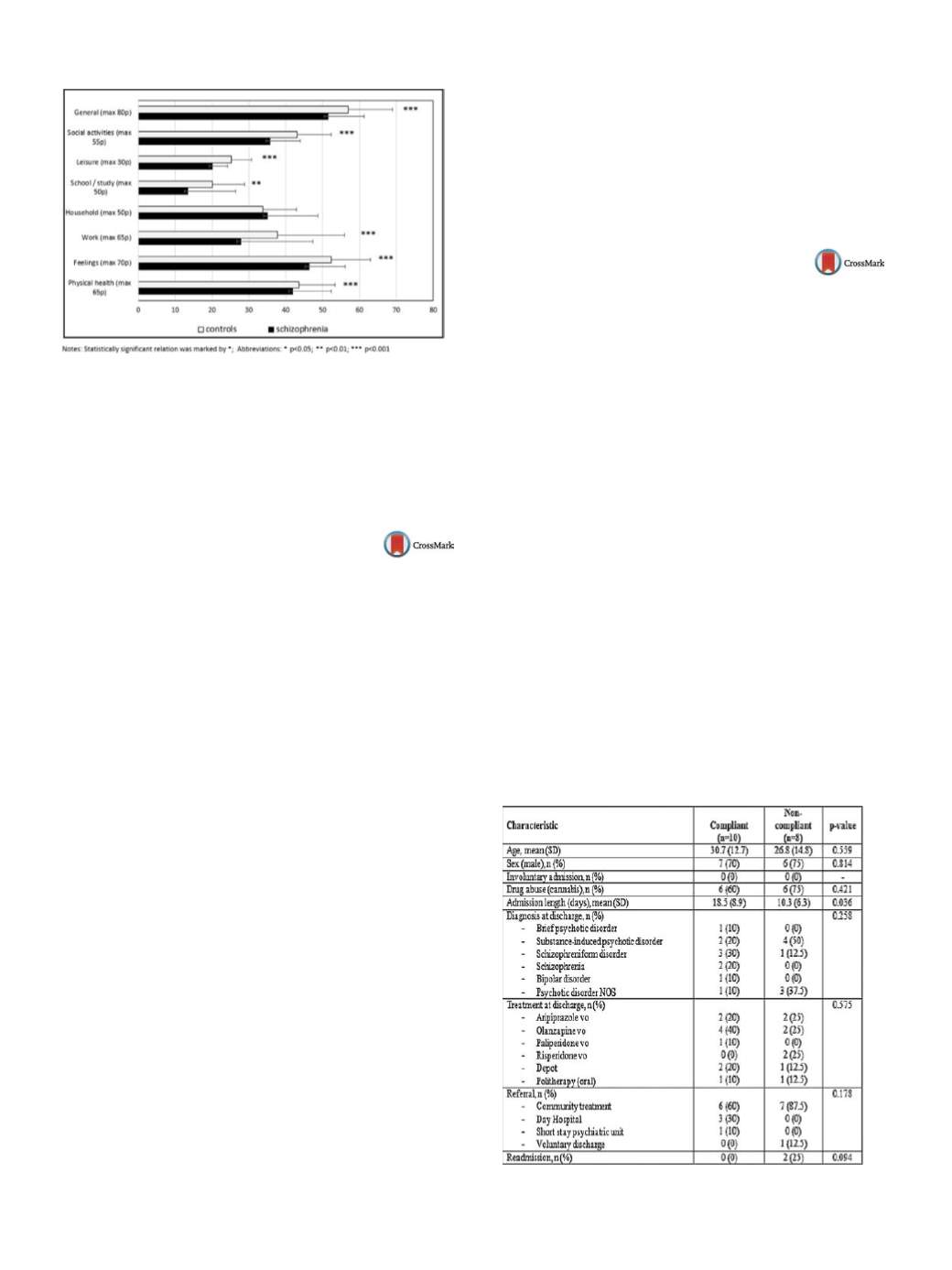
Fig. 1
Q-les-Q domains in the controls and the patients. Statis-
tically significant relation was marked by *. *
P
< 0.05; **
P
< 0.01;
***
P
< 0.001.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.642EW525
Cognitive function in early psychosis
patients from a low-income country
M.O. Husain
1 ,∗
, I.B. Chaudhry
2, T. Kiran
2, R. Thomasson
3,
N. Mehmood
4, N. Husain
21
Manchester mental health and social care Trust, general adult
psychiatry, Manchester, United Kingdom
2
University of Manchester, psychiatry, Manchester, United Kingdom
3
Penine acute care NHS Trust, psychiatry, Manchester, United
Kingdom
4
Pakistan institute of learning and living, research and development,
Karachi, Pakistan
∗
Corresponding author.
Background
Cognitive impairments are well established findings
in schizophrenia and are associated with significant impairment of
social functioning. Episodic memory, working memory and execu-
tive function test scores are typically 1 standard deviation below
healthy controls. There are reports suggesting the presence of neu-
rocognitive deficits prior to illness onset, opening the possibility
of using cognitive profiles as disease markers. Interest in exploring
cognitive functioning in early stages schizophrenia has continued
to grow, as earlier treatments could possibly lead to improved out-
comes.
Methods
This is a cross-sectional assessment of cognitive profiles
in patients with early psychosis. A total of 51 patients suffering
from psychosis in the age group of 18–65 years were recruited and
matched with 51 healthy controls. A wide range of neurocogni-
tive domains were assessed using standardised neuropsychological
tests.
Results
There was evidence of statistically significant impair-
ments in cognitive functioning across a broad range of cognitive
domains in early-psychosis patients, as compared to healthy con-
trols. More pronounced deficits were seen in executive function
tests.
Conclusions
To our knowledge, this is the first study to report
cognitive deficits across a range of domains in patients with first
episode psychosis from a low-income country. This study found
deficits across multiple domains, including language, memory,
attention, executive function, and visuospatial function in patients
with early psychosis. Evidence of neuropsychological deficits in
the early course of the disease may highlight crucial therapeutic
windows for both pharmacological treatments and cognitive reha-
bilitation. This may improve functional outcomes in this patient
group in the longer term.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.643EW526
Short-term compliance in
first-episode psychosis
N. Iriarte Yoller
1 ,∗
, J. Vicente Garcí
a 1 , F. Rico Villademoros
21
Hospital universitario de Burgos, psiquiatría, Burgos, Spain
2
Instituto de neurociencias, universidad de Granada, Granada, Spain
∗
Corresponding author.
Introduction
Non-compliance is a significant problem in patients
with first-episode psychosis (FEP), representing a challenge for
mental health professionals due to the heterogeneous course and
functional outcomes.
Objectives
The aimwas to describe the short-term compliance in
FEP and analyze the demographics, clinical features, and manage-
ment issues potentially associated with non-compliance.
Methods
This observational and retrospective study included all
consecutive FEP admitted to our psychiatry unit from January to
June 2015, belonging to our catchment area. To be categorized as
compliant, patients had to attend month-1 and month-3 follow-up
visits. Characteristics of compliant and non-compliant were com-
pared using a bivariate analysis.
Results
We included 18 patients whose characteristics are
shown in the table. Overall, 8 (44.4%) were non-compliant. Patients
who were non-compliant had a significantly shorter length of stay
(10.3 [6.3] vs. 18.5 [8.9] days). Most patients (66.7%) had cannabis
abuse, being slightly more frequent among non-compliant (75% vs.
60%,
P
=NS); in addition, the diagnosis of substance-induced psy-
chotic disorder was alsomore common among non-compliant (50%
vs 20%,
P
=NS). There were 2 patients who were readmitted, both
in the non-compliant group (Table 1).
Conclusions
Short-term non-compliance is high among patients
with FEP. Despite the limitations of our study, our results suggest
that, beside other factors (e.g. substance abuse), non-compliance
could be associated with management-related factors.
Table 1


















