
S294
24th European Congress of Psychiatry / European Psychiatry 33S (2016) S116–S348
EW513
Problems in long-term treatment
with atypical antipsychotics:
hyperprolactinemia
C. Franch
1 ,∗
, G. Medina
2, M.D. Ortega
3, M.E. Calzada
1,
V. Molina
21
Complejo Asistencial Universitario de León, Psiquiatría, Leon, Spain
2
Hospital Clínico Universitario de Valladolid, Psiquiatría, Valladolid,
Spain
3
Centro de Salud Mental Cartagena, Psiquiatría, Murcia, Spain
∗
Corresponding author.
Introduction
Schizophrenia and other psychotic disorders are
associated with high rates of morbidity and mortality, caused by
the use of specific treatments as well as health factors directly
related to those processes. One of the high-frequency side effects
in patients treated with classic and atypical antipsychotics is
hyperprolactinemia. It causes alterations in neuroendocrine sphere
(amenorrhea, galactorrhea, gynecomastia
. . .
), and other mid- and
long-term effects (osteoporosis, cardiovascular risk increase and
increased risk of developing cancers - specifically in breasts and
endometrium).
Objectives
Check hyperprolactinemia induction by maintained
treatment with atypical antipsychotics.
Methodology
A naturalistic prospective study was conducted fol-
lowing 75 patients onmaintenance treatmentwith a single atypical
antipsychotic during 24 months. Anthropometric and laboratory
datawere collected, alongwith the presence of different endocrine-
metabolic during the 2-year study alterations.
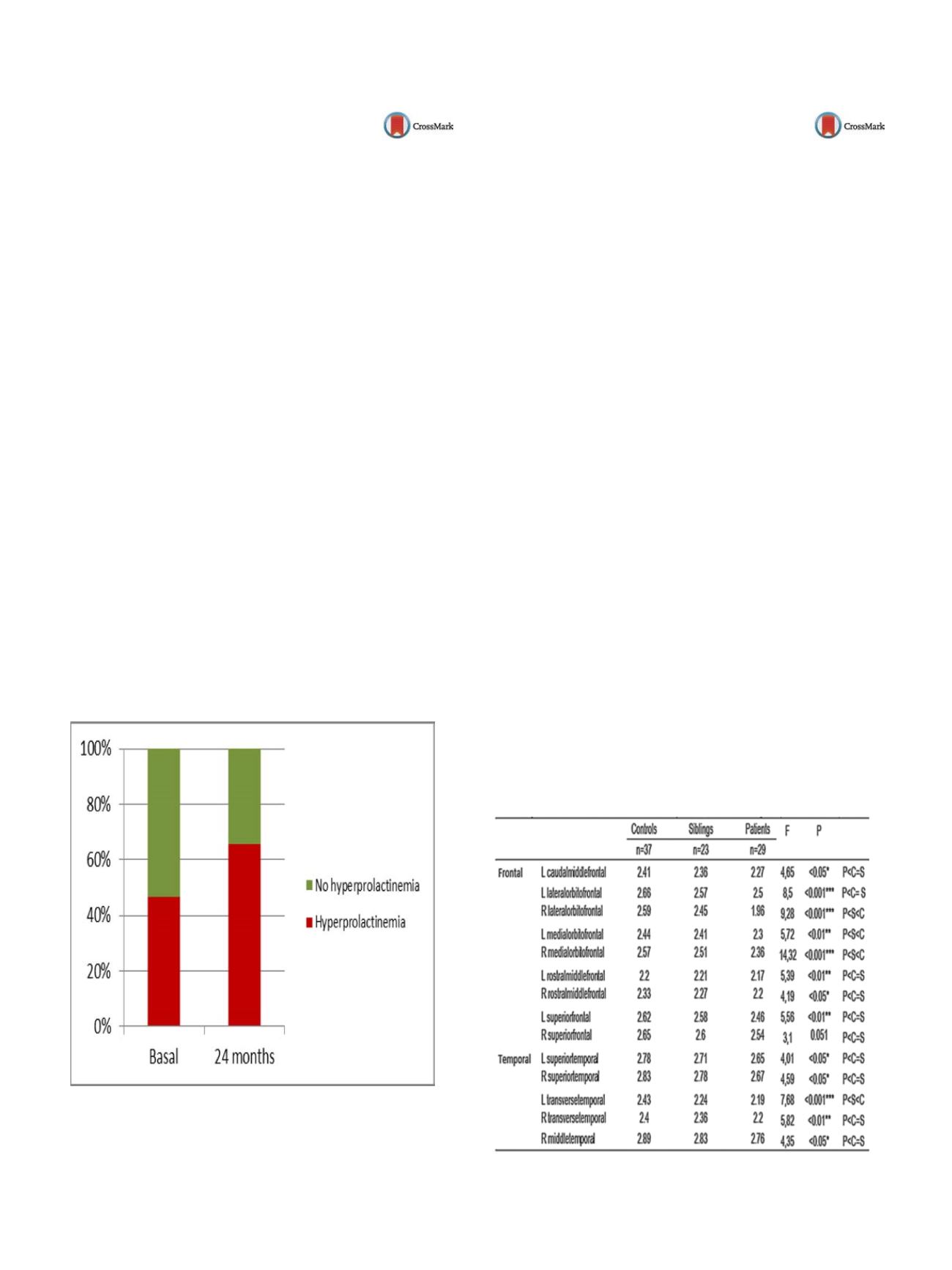
Results
Changes in prolactin levels were found in a large num-
ber of patients, with statistically significant differences between
0 (basal) and 24 months (Basal [M= 26.27; SD = 21], 2 years
[M= 38.08, SD = 34.65];
t
=
−
2.758;
P
= 0.013], with hyperpro-
lactinemia increasing from 46.6% of patients at baseline to 65.5%
at 2 years, mainly with paliperidone and risperidone long acting
injection (statistically significant increase in both cases)
( Fig. 1 ).Conclusions
Paliperidone and risperidone long acting injectable
induce increased prolactin levels in patients in long-term antipsy-
chotic treatment.
Fig. 1
Prolactine variation at 24 months.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.631EW514
Cortical and subcortical morphology
deficits in cerebral gray matter in
patients with schizophrenia and not
affected siblings
F. Pastoriza
1 ,∗
, L. Galindo
2, A. Mané
3, D. Bergé
3, N. Pujol
3,
M. Picado
4, A. Bulbena
2, O. Vilarroya
2, V. Pérez
51
IMIM - Universitat Autònoma de Barcelona, USM l’Hospitalet Nord-
ICS, Barcelona, Spain
2
Institut de Neuropsiquiatria i Addiccions - Parc de Salut Mar- IMIM-
Universitat Autònoma de Barcelona, Psychiatry, Barcelona, Spain
3
Institut de Neuropsiquiatria i Addiccions- Parc de Salut Mar- IMIM,
Psychiatry, Barcelona, Spain
4
IMIM, Neuroimaging, Barcelona, Spain
5
Institut de Neuropsiquiatria i Addiccions- Parc de Salut Mar- IMIM-
Universitat Autònoma de Barcelona, Psychiatry- CIBERSAM G21,
Barcelona, Spain
∗
Corresponding author.
Objective
Explore the basis of cortical morphometry in patients
with schizophrenia and non-affected siblings by Magnetic Reso-
nance Structural analyzing cortical thickness.
Methods
Twenty-nine patients with schizophrenia treated with
atypical antipsychotics and clinically stable in the last 6 months
were recruited. Twenty-three not affected siblings of patients with
schizophrenia and 37 healthy volunteers were recruited. Magnetic
Resonance Structural was performed. FreeSurfer the brain imag-
ing software package for analysis of Cortical Thickness is used. In
the analysis of group differences in cortical thickness (CT) with the
general linear model (GLM), the
P
-value was established in 0003
following the Bonferroni correction to control for multiple com-
parisons (seven regions of interest a priori in each hemisphere).
Results
Significant differences in cortical thickness between
patients and healthy controls. Differences between groups were
calculated by general linear model (GLM) with age and sex as cov-
airables
( Table 1 ).Conclusions
In applying the correction for multiple comparisons,
differences in bilateral-lateral orbitofrontal, medial orbitofrontal-
right and left temporal transverse frontal cortex are significant. Our
study replicates previous findings and provides further evidence of
abnormalities in the cerebral cortex, particularly in the frontal and
temporal regions, being characteristic of schizophrenia.
Table 1
Significant differences in cortical thickness in healthy con-
trols, not affected siblings and patients with schizophrenia.
P: patients; S: siblings; C: controls.


















