
24th European Congress of Psychiatry / European Psychiatry 33S (2016) S116–S348
S157
EW121
Nalmefene in alcohol use disorder
subjects with psychiatric comorbidity:
A preliminary report
M. Di Nicola
1 ,∗
, L. De Risio
1, M. Pettorruso
1, L. Moccia
1,
G. Martinotti
2, L. Janiri
11
Institute of Psychiatry and Psychology, Catholic University of Sacred
Heart, Rome, Italy
2
Institute of Psychiatry, Department of Neuroscience and Imaging,
“G. d’Annunzio” University of Chieti-Pescara, Chieti, Italy
∗
Corresponding author.
Introduction
Nalmefene is the first drug approved to reduce alco-
hol consumption in Alcohol Use Disorder (AUD) patients with a
high drinking risk level. There is a high prevalence of concurrent
psychiatric disorders in AUD patients, with an associated increased
morbidity and poorer prognosis.
Objectives
Despite high comorbidity rates, little attention has
been paid to the clinical management of these patients.
Aims
The aims of our studywere to evaluate the use of nalmefene
in AUD patients with psychiatric comorbidity, previously treated
unsuccessfully for alcohol dependence, and to assess reduction in
craving.
Methods
Thirty AUD outpatients (M/F: 19/11) with stabilized
anxiety and affective comorbid disorders were treated with as-
needed nalmefene 18mg plus psychosocial support for 24weeks.
Primary outcome measures were: changes in heavy drinking days
(HDDs) and total alcohol consumption (TAC, g/day). Secondary out-
come measures were: changes in Drinking Risk Level (DRL) and
craving levels (Obsessive-Compulsive Drinking Scale [OCDS] and
Visual Analogue Scale for craving [VASc]).
Results
The reduction of HDDs and TAC over time was significant
(
P
< 0.001). A decrease of DRL was reported. Moreover, a significant
reduction in craving levels was observed (OCDS and VAS crav-
ing scores,
P
<0.001). No patients dropped out of the study due to
adverse events.
Conclusions
As-needed nalmefene was well tolerated and useful
in reducing drinking in AUD patients with stabilized psychiatric
comorbidity that had not responded to previous interventions for
alcohol dependence. Nalmefene also reduced craving, which is
related to the motivation to consume alcohol.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.239EW122
Substance abuse and quality of life in
chronic hepatitis C patients receiving
antiviral treatment
E. Egmond
1 ,∗
, G. Oriolo
1, M. Cavero
1, K. Langohr
2, R. Solà
3,
R. Navines
1, R. Martin-Santos
11
Hospital Clínic, Psychiatry and Psychology, Barcelona, Spain
2
Polytecnic University of Barcelona, Statistics and Operation
Research, Barcelona, Spain
3
Hospital del Mar, Hepatology, Barcelona, Spain
∗
Corresponding author.
Introduction
Chronic hepatitis C virus (HCV) is one of world’s
most important chronic infections. HCV can be treated using
interferon-alpha (IFN ) and ribavirin (RBV). HCV, IFN and RBV
are known to impair mental and physical life quality. Many HCV-
infected individuals have life-prevalence of substance use disorder
(SUD).
Objectives
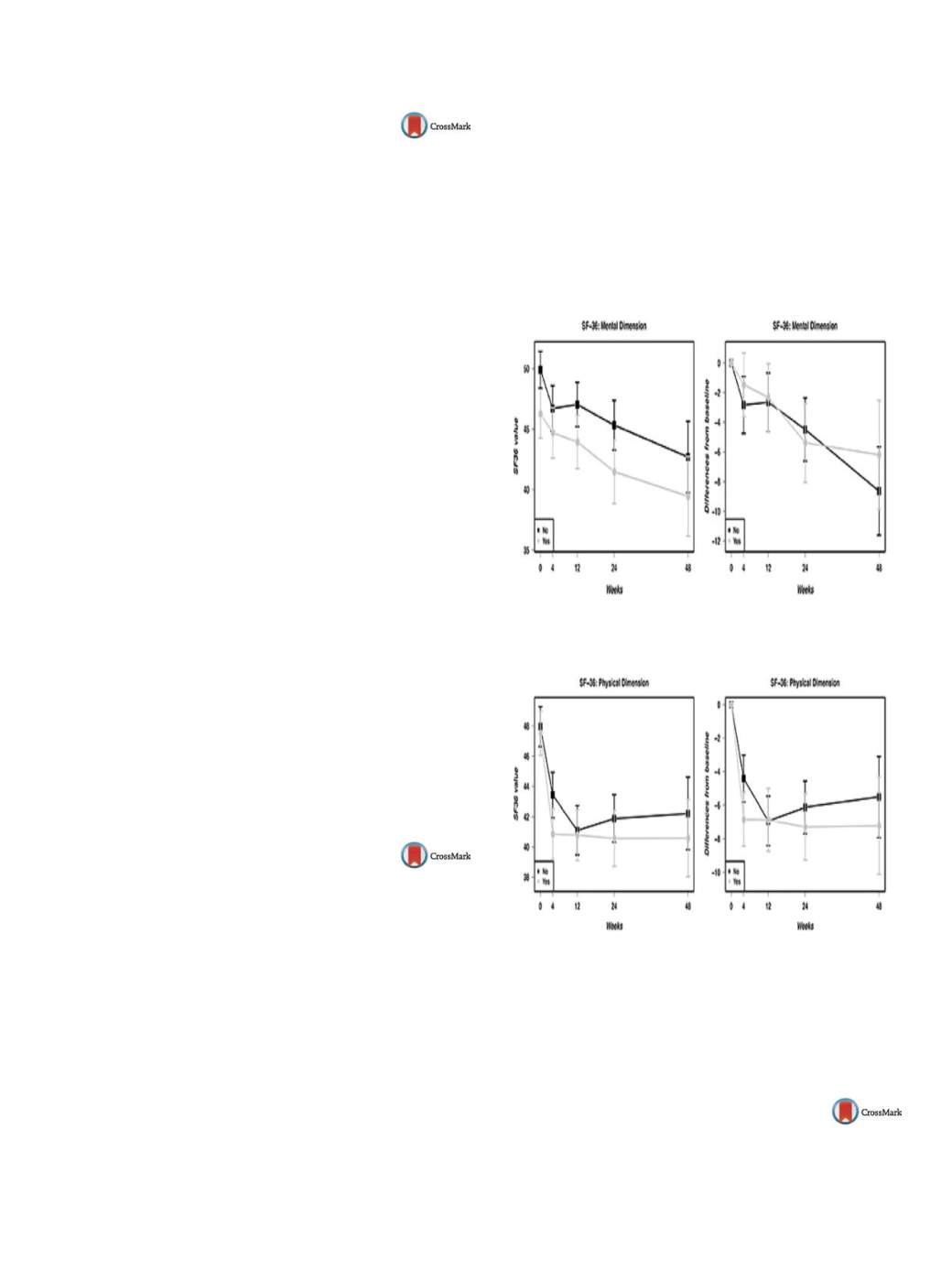
To study life quality (SF-36) in HCV patients with SUD
history during antiviral treatment.
Methods
SF-36 questionnaire was assessed in 384 HCV patients
at baseline, and at 4, 12, 24, and 48weeks of treatment. ANCOVA
models were used to study the association of SF-36 scores and
potential risk factors at baseline. Risk factors from baseline scores
over time were studied through linear mixed models, adjusting for
baseline scores.
Results
At baseline, SUD men had worse mental (
P
= 0.03) and
physical health (
P
= 0.022), and younger patients had worse social
functioning (
P
= 0.011), and mental (
P
= 0.001) but better physical
health (
P
< 0.001).
Figs. 1 and 2show the results of mental and
physical life quality during treatment from baseline.
Conclusions
This study emphasizes the decrease in life quality in
HCV patients with SUD before and during antiviral treatment.
Grant
Instituto de Carlos III-FIS: PSICOCIT-PI110/01827,EU “One
way to make Europe”, Ministerio de Economia y Competitividad
(MTM2012-38067-C02-01), and support of SGR/2014/1135.
Fig. 1
Mental component scale during treatment.
Fig. 2
Physical component scale during treatment. Adjusting for
gender, age, HIV co-infection, and history of mood disorders.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.240EW123
Challenging patients: Human misery
I. Ganhao
1 ,∗
, S. Paiva
2, J. Cardoso
21
Qta do Anjo, Portugal
2
Centro Hospitalar Psiquiatrico de Lisboa, Psiquiatria Geral e
Transcultural, Lisbon, Portugal
∗
Corresponding author.


















