
24th European Congress of Psychiatry / European Psychiatry 33S (2016) S349–S805
S367
2
Aarhus University Hospital, Psychiatric Research Academy,
Department of Affective Disorders, Risskov, Denmark
3
University of Southern Denmark, Department of Psychiatry, Odense
University Function, Odense, Denmark
4
Regional Psychiatry, Randers, Denmark
∗
Corresponding author.
Introduction
Physical comorbidities are common in patientswith
concurrent mental illness and substance use disorder. Interven-
tional studies addressing health promotion for this group of
patients are scarce.
Aims
To examine the physical health condition of a non-selected
group of patients with substance use disorder comorbid to other
psychiatric disorders. Further, to analyze for possible changes in
their health condition during a two-year intervention study in rela-
tion to physical measures and substance use. Finally, to analyze for
possible associations between changes in physical measures and in
substance use.
Methods
The patients were enrolled in the project continuously
from October 2013 through May 2015. Physical health measures
were obtained at the enrolment date and continuously as part of
daily clinical practice. Interventions consisted of individual consul-
tations with a research nurse, group sessions and an opportunity
to do physical exercise together with the research nurse. Interven-
tions included health promotion activities, i.e. guidance on healthy
food intake, smoking cessation and a physically active life.
Results
In total, 64 patients (mean age 32.7 years, SD 10.7) were
included in the study. Patients were mostly diagnosed with psy-
chotic disorders (11%), affective disorders (44%) or developmental
disorders (34%). Baseline measures showed that 89% of the patients
smoked cigarettes daily, 61% had used cannabis and 20% had used
amphetamines within the past month. Further, few patients did
moderate or vigorous physical exercise. Further results are in
progress.
Conclusions
These interventions seem relevant and manageable
in an outpatient setting.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.1039EV55
Delusional symptoms with alcohol
L. Montes Reula
1 ,∗
, A. Ballesteros Prados
21
Institute Salud Mental Gobierno Navarra, CHN Psychiatric,
Pamplona, Spain
2
Red Salud Mental Gobierno de Navarra, Mental health center,
Estella, Navarra, Spain
∗
Corresponding author.
A patient is twenty-eight years old who comes to the emergency
services because he has visual hallucinations related to alcohol con-
sumption. He only consumes alcohol sporadically in leisure time.
Since he began drinking at 18 years he has presented these symp-
toms in only four occasions. He does not relatewith amore quantity
of alcohol or another stressors. After a few minutes, these symp-
toms disappear and so he criticizes.
It is about of study through a clinical case the alcoholic hallucinosis,
their characteristics and to see the differences in the patient. The
patient in the acute phase presents a view of reality altered that
later he recovers. There is no loss of consciousness or behavioral
disorders. There are similarities with a pathological intoxication
but there is not a regular relationship between consumption and
symptoms.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.1040EV56
Do medical students use cognitive
enhancers to study? Prevalence and
correlates from lithuanian medical
students sample
A. Lengvenyt ˙e
1 ,∗
, R. Strumila
21
Lithuanian University of Health Sciences, Faculty of Medicine,
Kaunas, Lithuania
2
Vilnius University, Faculty of Medicine, Vilnius, Lithuania
∗
Corresponding author.
Introduction
Use of prescription psychostimulants and nootrop-
ics for non-medical purpose is a growing trend, especially in
academic environment. Seeing the risks of neuroenhancement we
decided to investigate situation in Lithuania.
Objective
Analyze the use of cognitive enhancers among medical
students in Lithuania.
Aims
1. Determine the prevalence of cognitive enhancement. 2.
Figure out what drugs are mostly used and reasons for the usage.
3. Evaluate the contributing factors.
Methods
A cross-sectional survey studywas performed in Vilnius
University and Lithuanian University of Health Sciences. Students
were asked to fill anonymous paper questionnaires consisting of 13
items concerning prevalence of substance use to enhance cognitive
performance, reasons, and correlates during lecture time.
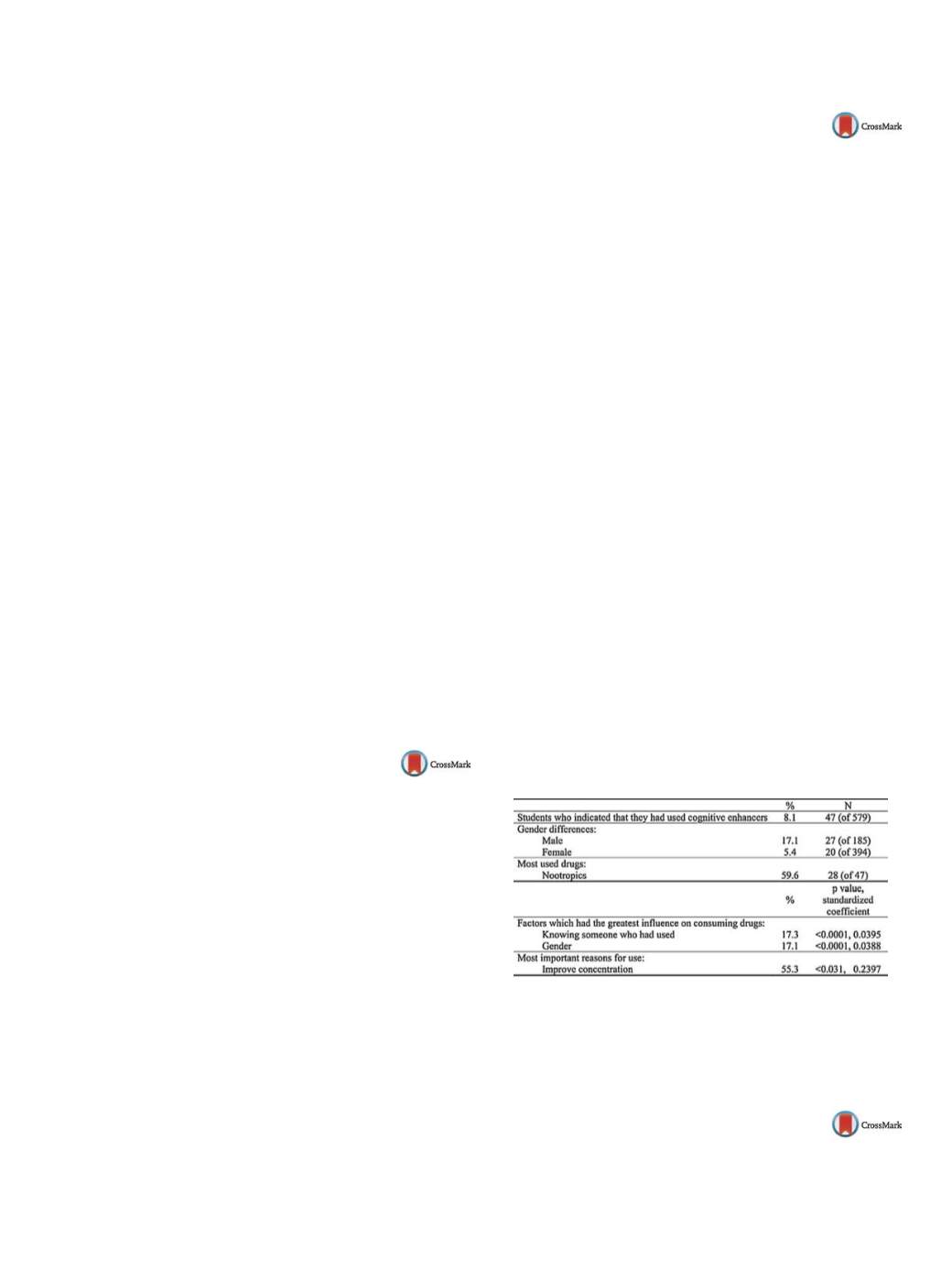
Results
Results are summarized in
Table 1 .A total of 8.1% of
responders indicated that they had used cognitive enhancers.
Nootropics were the most frequently mentioned: 59.6%, while psy-
chostimulants were mentioned less frequently: 38.3% (including
modafinil, methylphenidate and amphetamine derived drugs), and
23.4% indicated other substances. Improvement of concentration
and increased studying time were predominant purposes (55.3%
and 48.9% of users). Male students reported 3 times higher preva-
lence rates than females (14.6% vs. 5.1%,
P
< 0.05). Prevalence were
also higher in students, who knew someone using these substances
as compared to those who did not (17.3% vs. 5.1%,
P
< 0.05); it was
the most associated factor with cognitive-enhancing drug taking
behavior
( Table 1 ).Conclusions
In Lithuania, 1 of 12 medical students admits to hav-
ing used neuroenhancing drugs. Nootropics were the most used
drugs. Knowing user was the most important factor for usage.
Table 1
Main findings of this study.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.1041EV57
Exercise addicts with injuries are in
risk of depression
M. Lichtenstein
1 ,∗
, K. Andersen
2, U. Jørgensen
31
Department of Psychology, University of Southern Denmark, Odense
C, Denmark


















