
24th European Congress of Psychiatry / European Psychiatry 33S (2016) S349–S805
S445
3
Pitzer College, Psychology, Claremont-California, USA
4
Deparment of Mental Health, Juvenile Court Mental Health Service,
Monterey Park-California, USA
∗
Corresponding author.
Introduction
Telepsychiatry is increasingly utiilized to evaluate
and treat diagnostically and geographically diverse youth. (Szeftel
et al., 2012; Hilty et al., 2013). Important public health implications
arise for US psychiatrically ill youth, most of whomreceive no treat-
ment, others depend on pediatricians without input from a child
psychiatrist (Goldstein and Myers, 2014). Potential advantages of
telepsychiatry include increased access to care from child psychi-
atrists directly, and through collaborations with pediatricians, and
uniquely positive response in patients more communicative in this
setting (Pakyrek et al., 2010).
Objectives
– To present the effectiveness of Telepsychiatry in
psychiatrically ill youth, and specific subgroups who especially
benefit.
– To show increased access to psychiatric care occurs through col-
laborations between child psychiatrists and pediatricians.
Aims
To present the advantages of telepsychiatry for child and
adolescent mental health and clinicians.
Methods
Review of selected published Telepsychiatric evidence-
based research and best practice recommendations.
Results
– Psychiatrically ill youth are effectively evaluated and
treated using Telepsychiatry (Myers et al. (2011), Hilty et al., 2013).
– Very young children and youth with Autism SpectrumDisorders,
or anxiety disorders respond particularly positively to Telepsychi-
atry (Szeftel et al., 2012; Pakyuerek et al., 2010: Myers et al., 2010).
– Telepsychiatry provides increased access to care through collab-
orations between child psychiatrists and pediatricians (Goldstein
and Myers, 2014; Myers et al., 2011).
Conclusion
Telepsychiatry is a promising advantageous modality
for youth based on effectiveness, broad administration and unique
benefit for very young and socially impaired youth.
References not available.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.1288EV304
Management of psychiatric symptoms
in pediatric anti-NMDA receptor
encephalitis: Case report and
systematic review
S. Tang
∗
, O. Alpert
Children’s Hospital of Philadelphia, Child and Adolescent Psychiatry,
Philadelphia, USA
∗
Corresponding author.
Introduction
Anti-N-methyl-D-aspartate (NMDA) receptor
encephalitis is an autoimmune condition that causes serious psy-
chiatric symptoms. Nearly 40% of affected patients are pediatric in
age. Fewpublications detail management of psychiatric symptoms.
Objective
To guide clinical decision-making for psychiatrists
managing pediatric patients with anti-NMDA receptor encephali-
tis.
Aims
We present a systematic reviewof literature and an illustra-
tive case report of a 17-year-old girl who presented with psychosis,
agitation, and insomnia, and underwent treatment with olanzap-
ine, clonazepam, and clonidine.
Methods
PUBMED was searched for publications in English
describing anti-NMDA encephalitis (2007–November 2015). Pub-
lications were included if they met all of the following:
– novel data;
– reported treatment of psychiatric phenomena for patients aged
≤
18 years
– full text available. Thirty-four publications detailing 38 unique
cases were included.
Results
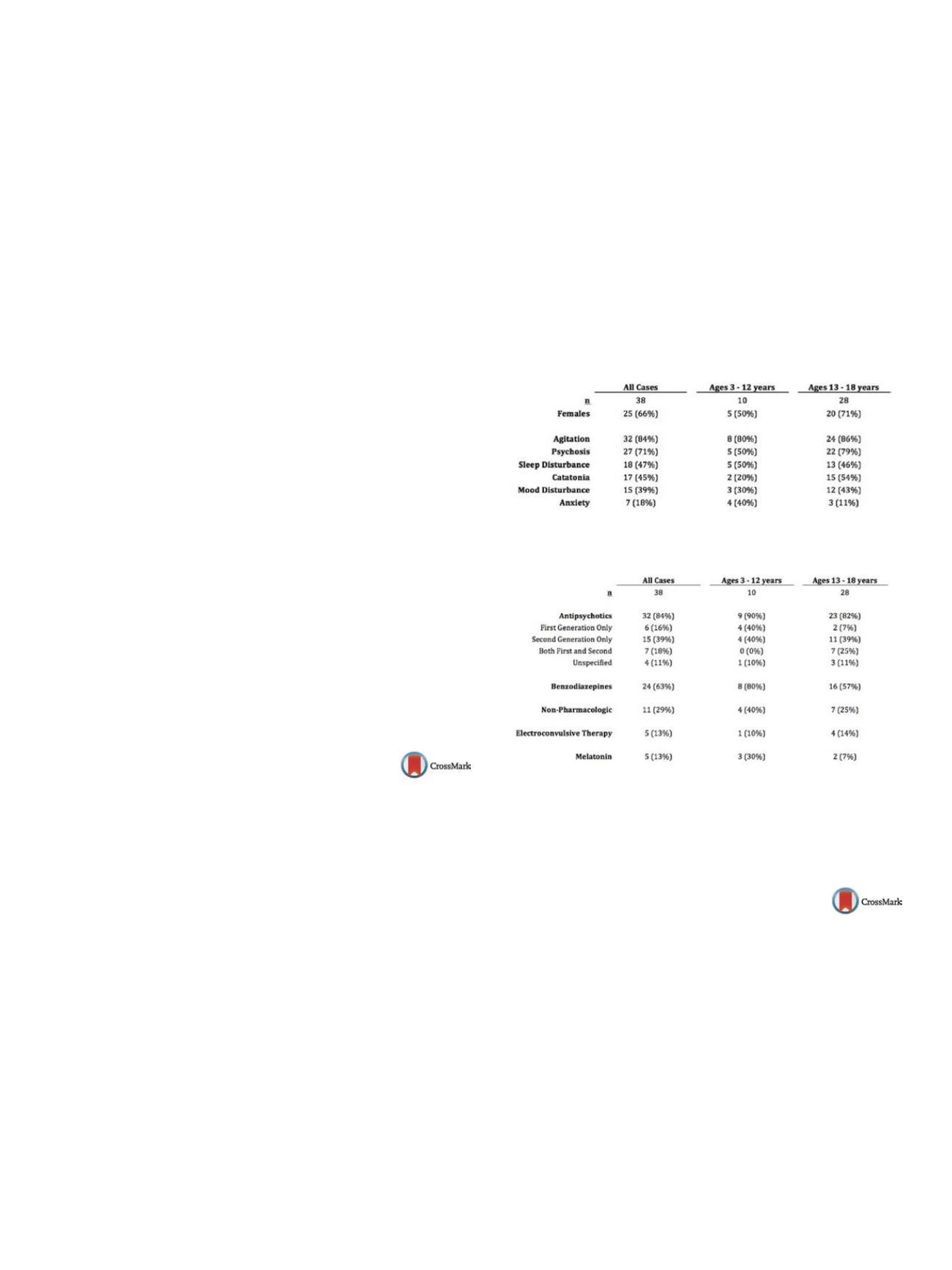
Psychiatric symptoms are summarized in
Table 1 ;com-
mon treatment modalities are presented in
Table 2 .The most
frequently used antipsychotics were risperidone (
n
= 16, 57%),
haloperidol (
n
= 10, 36%), and olanzapine (
n
= 10, 36%). Significant
adverse effects occurred, with neuroleptic malignant syndrome
diagnosed with high probability in 4 cases (13%), and suspected
in 5 cases (16%). Dystonia, rigidity, tremors, and bradykinesia were
also linked to medication side effects. All reported adverse events
coincided with antipsychotic administration.
Conclusions
Psychiatric symptoms in pediatric cases of anti-
NMDA receptor encephalitis were frequently managed with
antipsychotics and benzodiazepines. Though antipsychotics may
be necessary, serious side effects are concerning. Unlike in delir-
iumresulting fromother causes, benzodiazepines do not seemto be
contraindicated. ECT may also be of utility and was well-tolerated
in reported cases.
Table 1
Summary of psychiatric symptoms.
Table 2
Management of psychiatric symptoms.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.1289EV305
Feasibility of the stress and anger
management program on children
with high functioning autism
spectrum disorder in a sample
population from Karachi
B. Tauseef
∗
, Z. Zadeh , B. Fatima
Bahria University, Institute of professional Psychology, Karachi,
Pakistan
∗
Corresponding author.
Introduction
Research shows that individuals with Autism Spec-
trum Disorder, struggle with emotional competence as compared
to their typically developing counterparts. This leads to internal-
izing (stress) and externalizing (anger management) problems in
the affected population. The stress and anger management pro-
gram (STAMP) designed by Scarpa et al. is a manualized treatment
protocol with good clinical efficacy.
Objective
The objective of the present study is to test the feasibil-
ity and suitability of STAMP as a systematized treatment protocol


















