
24th European Congress of Psychiatry / European Psychiatry 33S (2016) S116–S348
S257
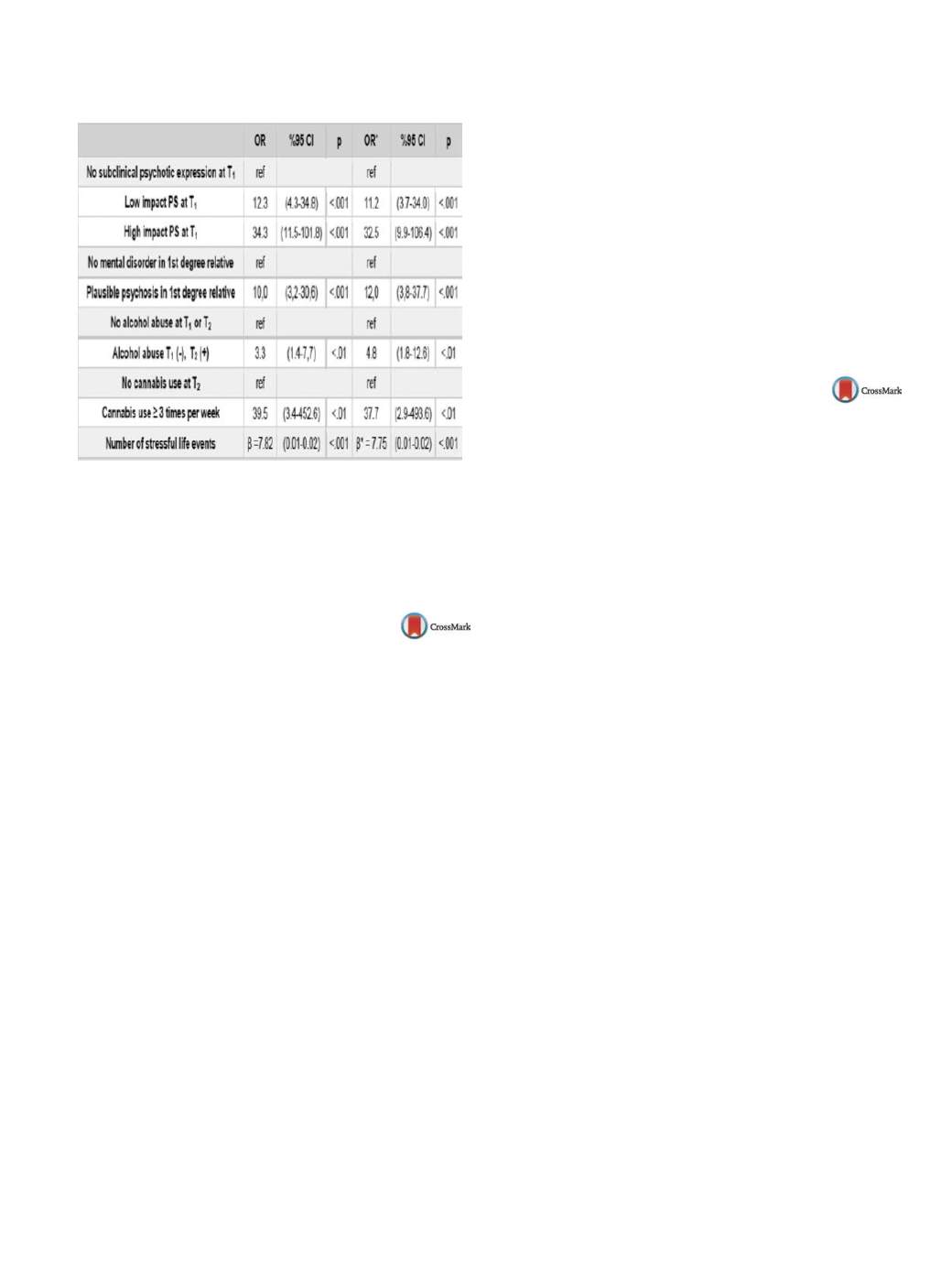
Table 1
Associations between independent variables and newly
onset clinical psychosis at
T
2
.
*
Adjusted for age, sex, education level and health insurance
status.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.526EW409
Perceived stigma in patients affected
by psychosis: Is there an impact on
relapse?
L. Sideli
1, F. Seminerio
2 ,∗
, M.V. Barone
1, A. Mulè
1, C. La Cascia
1,
C. Sartorio
1, R. D’Agostino
1, L. Ferraro
2, G. Tripoli
3,
A. Francomano
1, M. Inguglia
4, G. Vassallo
4, C. Majorana
4,
D. La Barbera
11
Università degli Studi di Palermo, Biomedicina Sperimentale e
Neuroscienze Cliniche BioNeC, Palermo, Italy
2
Università degli Studi di Palermo, Dipartimento Biomedico di
Medicina Interna e Specialistica DIBIMIS, Palermo, Italy
3
King’s College of London, Psychology and Neuroscience, London,
United Kingdom
4
Azienda Sanitaria Provinciale 6, Salute mentale e dipendenze
patologiche, Palermo, Italy
∗
Corresponding author.
Introduction
The World Health Organization (WHO) considers
stigma of mental illness as a crucial problem (WHO, 2001). Stigma
contributes to the onset (Morgan et al., 2010) and the outcome of
people affected by schizophrenia (Himan, 2015).
Objectives
To evaluate the perception of patients affected by psy-
chotic disorders of being stigmatized by the community.
Aims
To compare the perception of stigma among subgroups of
patients at different stage of their disorder.
Methods
Thirty-five patients affected by a first-episode of psy-
chosis (FEP) and 96 patients affected by chronic psychosis were
recruited. The Devaluation of Consumers Scale (DCS) and the Deval-
uation of Consumer Families Scale (DCFS) were administered to
assess the perceived public stigma (Struening et al., 2001). The Pos-
itive And Negative Schizophrenic Symptoms Scale (PANSS) (Kay
et al., 1987) and the Global Assessment of Functioning (GAF) (Gold-
man et al., 1992) were administered to assess psychotic symptoms
and global level of functioning.
Results
Patients affected by chronic psychosis perceived higher
devaluation against mental disorders than patients with a
recent onset of psychosis (Mann–Whitney’s
U
= 910.500,
P
= 0.017).
DCS and DCFS correlated with increased voluntary admis-
sions (Rho = 0.355,
P
= 0.002; Rho = 0.257,
P
= 0.029) and DCS with
increased compulsory admissions (Rho = 0.349,
P
= 0.003). Only
among chronic patients, DCS factor 2 was related to global level
of functioning (Rho = 0.217,
P
= 0.041).
Conclusions
Patients affected by chronic psychotic disorders
perceived a more pessimistic attitude of the community towards
their participation in social and community life and this is related
to increased admissions and disability.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.527EW410
Early detection and treatment of
mental illness in the workplace –
an intervention study
H. Sørensen
1 ,∗
, J. Valentin
1, M.K. Bording
1, J.I. Larsen
2,
A. Larsen
2, Ø. Omland
31
Aalborg University Hospital, Unit for Psychiatric Research, Aalborg,
Denmark
2
Aalborg University Hospital, Psychiatric Hospital, Aalborg, Denmark
3
Aalborg University Hospital, Occupational Medicine, Aalborg,
Denmark
∗
Corresponding author.
Introduction
Conditions of depression and anxiety among
employees’ leads to increased absenteeism and decreased social
and professional function.
Objectives
To test a collaborative model for contributing to men-
tal health at work at the lowest interference and highest possible
availability among Danish workers.
Aims
To investigate the effect of early detection and treatment
in order to interrupt and improve conditions of clinical and sub-
clinical levels of mental illness.
Methods
Self-reporting questionnaires were used for identifi-
cation of clinical and sub-clinical cases of mental illness and for
follow-up. Four questionnaires were distributed to all employees
in six medium-large companies in Denmark (
n
= 1292) during a
period of 16 months. Employees meeting the screening criteria
were assessed diagnostically. Outpatient psychiatric treatment was
offered to employees diagnosed with mental illness and preven-
tive CBT-session to those assessed with sub-clinical conditions.
Follow-up questionnaires were filled out after 6 and 12 months.
Data were analysed using repeated measure mixed effects linear
regression.
Results
Of the 587 (55%) employees that returned the question-
naires, 58 were referred to either outpatient psychiatric treatment
(
n
= 38) or preventive treatment (
n
= 20). Levels of psychopathology
decreased significantly in both treated groups. Comparing with the
pre-treatment period, a significant positive difference in change in
psychopathology was detected for employees in psychiatric treat-
ment. Measured up to healthy controls, the self-perceived level of
stress also decreased significantly among employees in psychiatric
treatment.
Conclusions
An integrated collaborative model for early detec-
tion and treatment was beneficial in order to interrupt and improve
the course of mental health problems among Danish employees.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.528

















