
S720
24th European Congress of Psychiatry / European Psychiatry 33S (2016) S349–S805
course of this disease. This process emphasizes all the cognitive
as both individual capacities as motor through an approach to
vocational, residential, recreational, social and educational support,
tailored to the unique demands of the patient, in every situation and
custom mode.
For this, working through concepts such as social cognition and
insight, interdisciplinary way, so to SET goals and accomplish them
with a specific planning.
Schizophrenia is a chronic disease that occurs in 1 to 2% of theworld
population, and causes social marginalization and stigmatization
in patients who have it. Be treated, then, since the integration of
multidimensional therapeutic resources.
In this paper, descriptively explains the techniques and activities
developed individually for each professional and interdisciplinary
area of building situational and individual patient diagnosis, poten-
tial and limitations as well as the specific treatment that may lead
to improved cognitive and motor skills of the patient, and from it
an improvement in their social inclusion and quality of life.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.2146EV1162
Effect of switching to long-acting
injectable (LAI) aripiprazole on
long-lasting antipsychotic-induced
hyperprolactinemia: A report of two
cases
M. Juncal Ruiz
∗
, B. Fernández-Abascal Puente ,
R. Landera Rodríguez
Hospital Universitario Marqués de Valdecilla, Psychiatry, Santander,
Spain
∗
Corresponding author.
Introduction
Antipsychotic-induced
hyperprolactinemia
(> 29 ng/ml in women) is associated with relevant side-effects.
Aim
We describe the case of two women aged 50 and 54 years,
respectively, diagnosed with schizophrenia who were receiving
outpatient treatment with paliperidone depot 100mg/month and
risperidone depot 50mg/2weeks, respectively and complained of
oligoamenorrhoea and amenorrhoea for at least 6months.
Methods
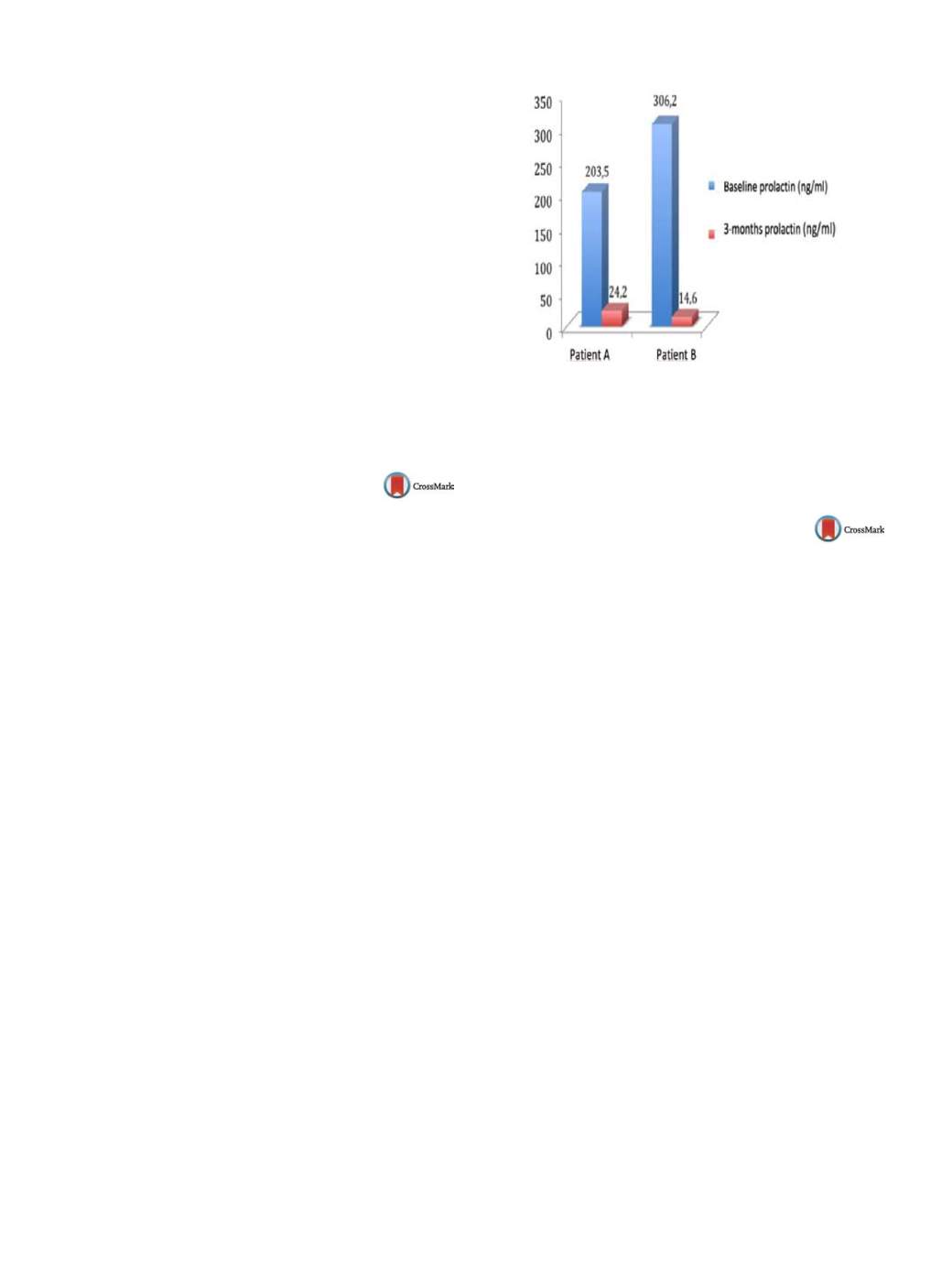
Routine blood tests showed hyperprolactinemia of
203.5 ng/ml and 306.2 ng/ml, respectively. The patients were eval-
uated by the Endocrinology unit and an MRI was performed
discarding the presence of any primary brain condition. Both
patients were switched to LAI aripiprazole due to its partial ago-
nism of D2-brain receptors. At the time of switching both patients
were stable in terms of psychopathology.
Results
Changes in prolactin levels 3months after switching are
shown in the
Fig. 1 .Two months after switching, both patients
regained cyclic menstrual function. After 6months, they still
showed psycopathological stability.
Conclusions
Several studies have described an improvement of
drug-induced hyperprolactinemia after switching to or adding oral
aripiprazole. In these two cases, the normalization of prolactin
levels and the resolution of oligoamenorrhoea/amenorrhoea were
observed as soon as 2–3months after switching to LAI aripiprazole.
These findings suggest that switching to LAI aripiprazole may be
an effective alternative for managing antipsychotic-induced hyper-
prolactinemia.
Fig. 1
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.2147EV1163
Capgras-delusion in a female patient
with schizophrenia: A case report and
study of the literature
P. Kolarov
1 ,∗
, P. Chumpalova
1, G. Georgiev
1, A. Todorov
2,
M. Stoimenova
11
Medical University, Pleven, Bulgaria, Department of Psychiatry and
Medical Psychology, Pleven, Bulgaria
2
University Hospital, Pleven, Bulgaria, Psychiatry Clinic, Pleven,
Bulgaria
∗
Corresponding author.
Background
The Capgras syndrome is a rarely observed condition
in patients with different psychiatric diseases, which is character-
ized with delusional misidentification of people, places, objects,
etc.
Objective
In this case report we aim to describe the clinical char-
acteristics and manifestation of Capgras syndrome in a female
patient with schizophrenia, performa literature search on the topic
and compare our report to literature findings.
Results and discussion
A 50-year-old female patient was verbally
and physically aggressive to her family members upon admis-
sion to our center. The onset of disease was marked 2 years ago
when she first started feeling deserted and isolated and had a pre-
scribed therapy for her condition which she did not follow. During
the current admission a psychiatric assessment was performed.
Delusional misidentification of her family members was observed
and consequent food and sleep self-deprivation due to psychosis
was noted. The patient denied being suicidal but was intense and
psychotic, and reported different objects to have started disap-
pearing mysteriously from her home. The patient was diagnosed
with schizophrenia and was treated with haloperidol, olanzapine,
chlorpromazine, and biperiden. The patient was discharged in an
improved condition, without episodes of obsessive delusions and
improved communication with her relatives.
Conclusion
Although according to the literature organic substrate
may be found in some patients with Capgras syndrome, in the case
presented here it is the dominant psychotic theme, which deter-
mined the content of the disease.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.2148

















