
24th European Congress of Psychiatry / European Psychiatry 33S (2016) S349–S805
S405
Results
The mean age was 30 years. Bipolar disorder type I
accounted for 72.5%.
According to the SBQ, 37.5% of patients had a desire disorder, 57.5%
had a frequency less than 3 times per week sexual intercourse, 45%
had a drop in excitation and 42.5% were not satisfied with their sex
life.
Sexual problems are positively correlated at an early age of onset
of bipolar disorder (
P
= 0.001).
The lack of desire, the sexual excitation disorder and the decrease in
the frequency of sexual intercourse are positively correlated with
the depressive phase of bipolar disorder.
Conclusion
A better understanding of sexual behavior in women
with bipolar disorder and the early screening of the sexual disor-
ders must be integrated into the management of the disease. It can
improve their quality of life and adherence to therapy.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.1157EV173
Dealing with bipolar disorder
H. Guillen Rodrigo
∗
, R. Remesal Cobreros ,
R. Alonso Díaz
Hospital Juan Ramon Jimenez, Salud Mental, Huelva, Spain
∗
Corresponding author.
The psychoeducational group therapy program for patients diag-
nosed with bipolar disorder is carried out in the Hospital Vazquez
Diaz in Huelva. The objectives of the group therapy are: provide
an adequate patient awareness of the disease, improve the drugs
adherence, facilitate early detection of new episodes, stress man-
agement, avoid the use and abuse of illegal substances, achieve a
consistency in their lifestyle, prevent suicidal behavior, increase
understanding and coping with the psychosocial consequences of
the past and future episodes, improve social activity, cope with the
subsyndromal residual symptoms and the following deterioration
and increase the welfare and the quality of life.
The group consists of patients diagnosed with bipolar disorder I, II
and cyclothymia. The psychiatrist has to establish if it is convenient
for the patient to attend the group and has to communicate, if it
has been detected, lack of knowledge about the disease, distorted
beliefs, lack of awareness of the disease, unhealthy habits and poor
adherence to the treatment.
The group was a closed group consisting of 10 to 12 patients. It was
carried by a clinical psychologist with the help of the clinical psy-
chology residents. The psychoeducational program we developed
in our hospital consisted in 9 bimonthly sessions of 90minutes.
As a result, we can say that the psychoeducation was very useful
in improving the course of bipolar patients and in reducing the
number of episodes and hospitalizations. Patients who received
psychoeducation and pharmacotherapy have suffered significantly
fewer relapses. Therefore, there is a prophylactic efficacy of psy-
choeducation in bipolar disorders.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.1158EV174
An fMRI study in patients with active
mania using Verbal N-Back test
R. Gupta
1 ,∗
, P. Goyal
1, R. Ranjan
1, S. Kumaran
2, R. Sagar
11
All India Institute of Medical Sciences, Psychiatry, New Delhi, India
2
All India Institute of Medical Sciences, Nuclear Magnetic Resonance,
New Delhi, India
∗
Corresponding author.
Introduction
There is a lack of consensus on the dysfunctional
brain areas underlying mania.
Aims and objectives
The study was carried out to understand the
various brain networks implicated in active mania.
Methods
After obtaining ethical clearance from the Institute
Review Board, we recruited 30 subjects with active mania and 15
healthy controls using purposive sampling, and applying SCID. A
computerized cognitive test (Verbal N-Back) was used.
Results
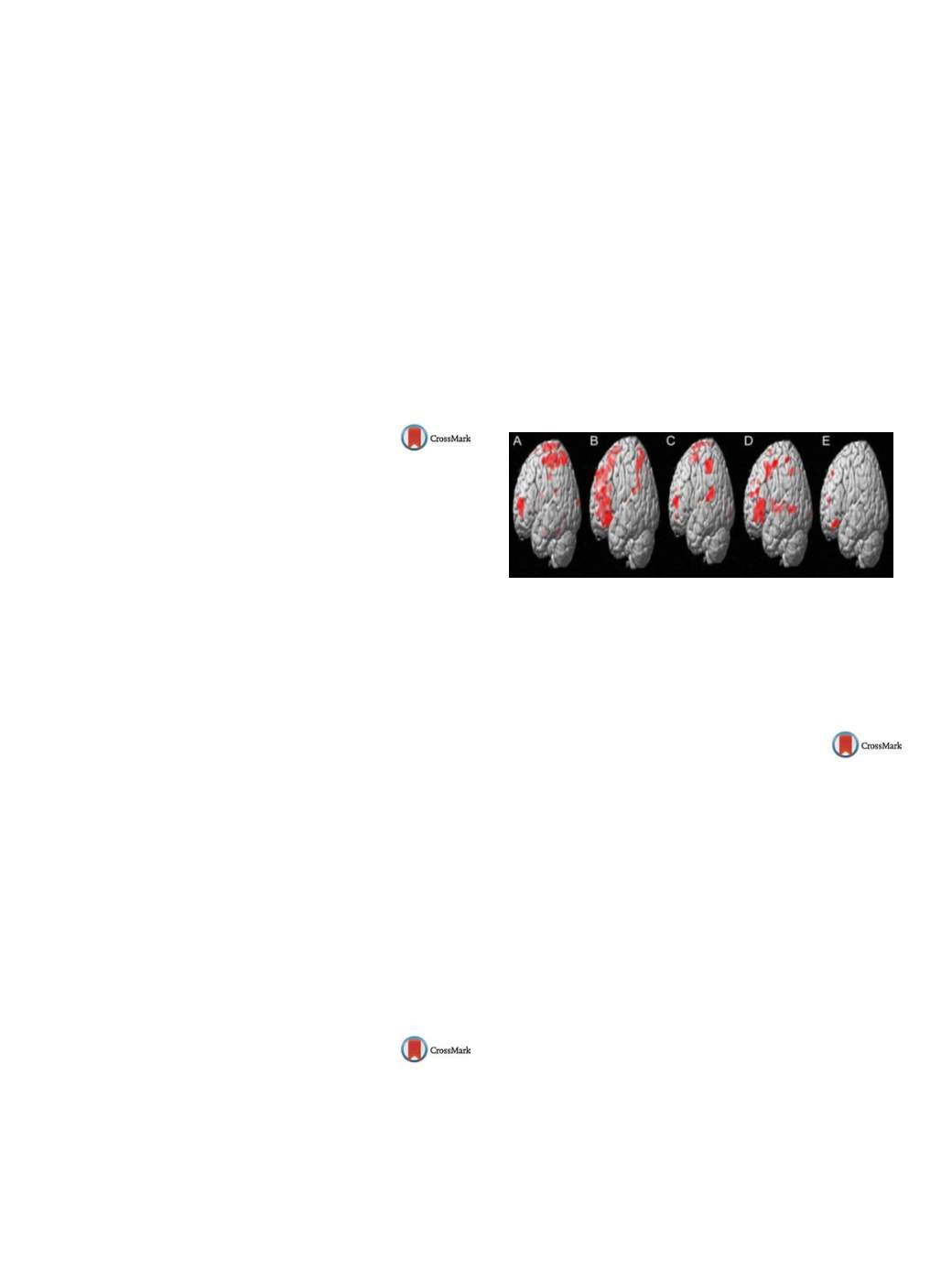
Mania group took significantly longer time while mak-
ing correct responses. They
( Fig. 1 C) showed activation in bilateral
frontal lobe, and bilateral superior temporal gyrus during verbal
1-Back task, whereas, the control group
( Fig. 1 A) showed left mid-
dle frontal gyrus, and right superior frontal gyrus activation. On
verbal 2-Back task, the mania group
( Fig. 1 D) had bilateral frontal
lobe, and bilateral superior temporal gyrus activation, whereas the
control group
( Fig. 1 B) had activation in the bilateral frontal lobe.
Conclusions
It was clearly visible that the mania group was sig-
nificantly slower in giving correct responses on N-Back task as
compared to the controls. On the 2-Back task, there was under-
activation in left frontal lobe in the mania group with respect to
the control group
( Fig. 1 E). This implies that the mania group may
have deficits in information processing speed.
Fig. 1
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.1159EV175
Self-stigma, treatment adherence, and
medication discontinuation in
patients with bipolar disorders in
remission – a cross-sectional study
M. Hajda
∗
, D. Kamaradova , J. Prasko
University Hospital Olomouc, Klinika psychiatrie, Olomouc, Czech
Republic
∗
Corresponding author.
Introduction
Self-stigma is a gradual process during which a
stigmatized person uncritically accesses and integrates negative
societal stereotypes towards persons with mental disorders.
Objective
It has been repeatedly shown that fear of stigma and
self-stigma is associated with lower adherence to various medical
procedures.
Aims
The aim of study is to investigate the relationship between
current adherence, discontinuing of medication in the past and self-
stigmatization by stable patients with bipolar disorder.
Method
Until now 33 outpatients with bipolar disorder com-
pleted The Drug Attitude Inventory-10 items (DAI-10) scale used
to estimate adherence to treatment, the Internalized Stigma Men-
tal Inventory scale (ISMI) measuring self-stigma and The Clinical
Global Impression (CGI), which assesses current severity of mental
disorders. Demographic and clinical data were also obtained.
Results
Current results show that, the level of adherence to phar-
macotherapy positively correlated with age and negatively with
self-stigma. Nineteen (57.6%) patients discontinued medication at
least once in the past. The patients, who discontinued medica-
tion in the past, were significantly younger and more often single


















