
S176
24th European Congress of Psychiatry / European Psychiatry 33S (2016) S116–S348
EW177
Government employees and
depressive and anxiety disorders:
A systematic review
M.A. Dos Santos
Porto, Portugal
Introduction
Depressive and anxiety disorders are common
among working adults and costly to employers and individuals
and their prevalence is high. Public sector employees are also vul-
nerable to poor mental health, mainly where have been occurring
organisational changes similar to private sector concepts.
Objective
To highlight the unmet mental needs for new vulnera-
ble working population, government employees.
Methods
The searchwas conducted using PubMed, Medline,Web
of Science, Scopus, B-on, Science Direct with the terms “gov-
ernment employees”, “federal employees”, “depressive disorders”,
“anxiety disorders”. Using the PRISMA methodology, 1374 articles
were considered with the search terms and if were published in
the last 10 years; after a review of the title and summary, 5 eligible
studies in english were included.
Discussion
Mental disorders are growing public health problem,
and creating an enormous toll of suffering, disability and economic
loss. There are few studies about depressive and anxiety disorders
in public sector and those confirm that it would be to examine to
what extent national characteristics can explainwhy individual and
organizational characteristics are more related to them in some
countries than in others, especially not including military or police
officers who usually are submitted to high psychological distress.
Conclusions
Workplace healthpromotion in addressing job stress
is crucial to fight against to a range of mental health outcomes.
Mental health screening in the public sector may contribute for
changes to the traditional roles of government and its manage-
ment structures andmust be encouraged to find out the underlying
mechanisms of developing depressive and anxiety disorders.
Disclosure of interest
The author has not supplied his/her decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.295EW178
Decentering and avoidance:
Mechanisms between external shame
and depression symptomatology
C. Ferreira
∗
, A.L. Mendes , J. Marta-Simões , I.A. Trindade
Faculty of Psychology and Educational Sciences - University of
Coimbra, CINEICC - Cognitive Behavioural Centre for Research and
Intervention, Coimbra, Portugal
∗
Corresponding author.
It is widely accepted that shame plays a significant role in the
development and maintenance psychopathology, namely depres-
sive symptoms. In fact, the experience of shame is highly associated
with the adoption of maladaptive strategies to cope with nega-
tive feelings, such as experiential avoidance (i.e., the unavailability
to accept one’s private experiences), and the inability of decen-
ter oneself from unwanted internal events. The present study
aims to explore a mediation model that examines whether exter-
nal shame’s effect on depressive symptomatology is mediated
through the mechanisms of decentering and experimental avoid-
ance, while controlling for age. Participants were 358 adults of
both genders from the general population that completed a bat-
tery of self-report scales measuring external shame, decentering,
experimental avoidance and depression. The final model explained
33% of depression and revealed excellent model fit indices. Results
showed that external shame has a direct effect on depressive
symptomatology and simultaneously an indirect effect mediated
by the mechanisms of decentering and experiential avoidance.
These data seem to support the association between shame and
depressive symptomatology. Nevertheless, these findings add to
literature by suggesting that when the individual presents higher
levels of shame he or she may present lower decentering abilities
and tends to engage in experiential avoidance, which amplify the
impact of external shame and depression. Furthermore, our find-
ings seem to have important clinical implications, stressing the
importance of developing intervention programs in the community
that target shame and experimental avoidance and that promote
adaptive emotion regulation strategies (e.g., decentering) to deal
with adverse experiences.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.296EW179
Chronic illness-related shame and
experiential avoidance mediate the
impact of IBD symptomatology on
depression
I.A. Trindade , C. Ferreira
∗
, J. Pinto-Gouveia
Faculty of Psychology and Educational Sciences - University of
Coimbra, CINEICC - Cognitive Behavioural Centre for Research and
Intervention, Coimbra, Portugal
∗
Corresponding author.
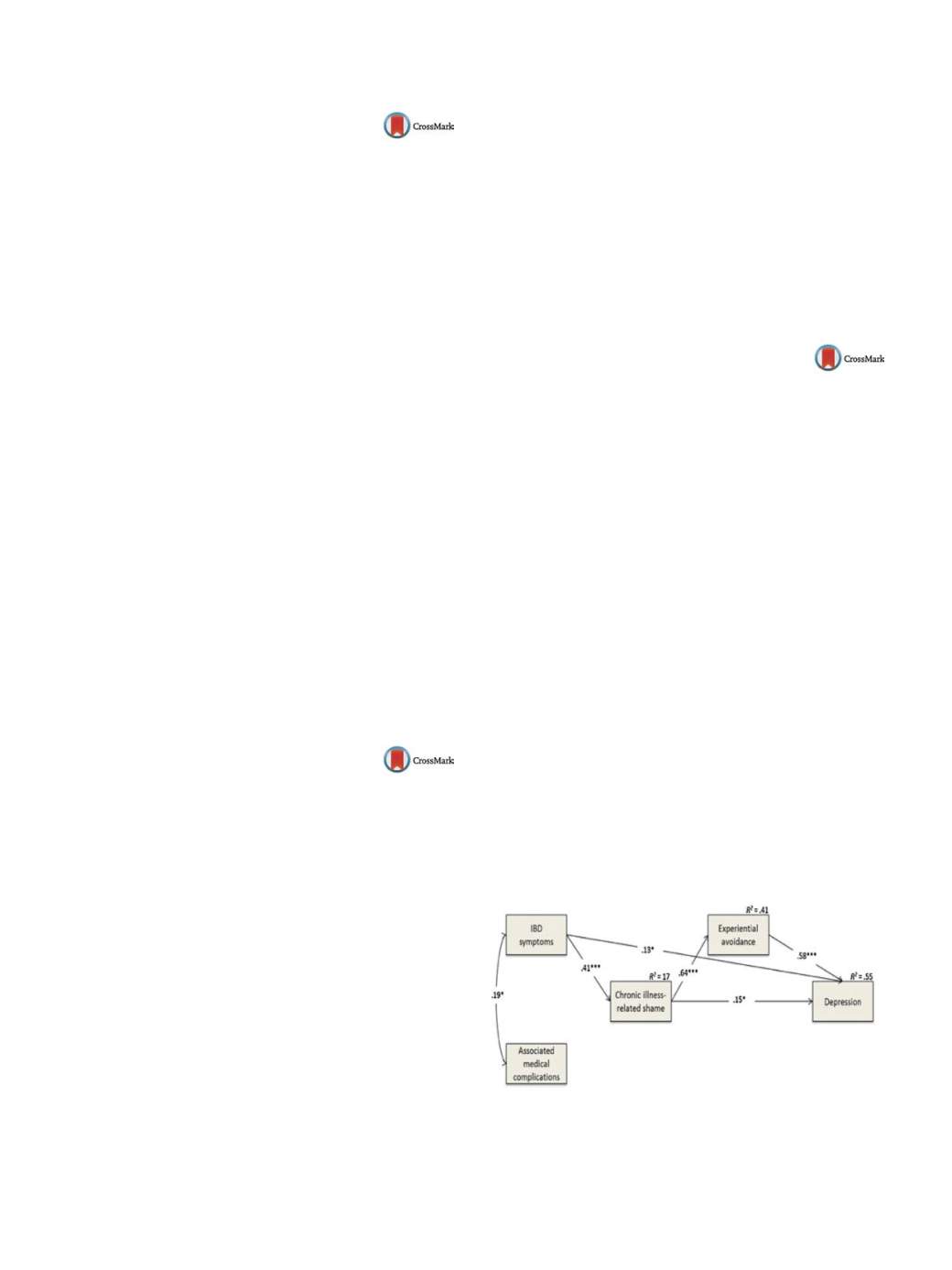
Inflammatory bowel disease (IBD) is group of chronic diseases that
cause symptoms such as abdominal pain, urgent diarrhoea and
fatigue, as well as associated complications (e.g., arthritis). Liter-
ature has pointed that IBD may cause depressive symptomatology,
which seems to aggravate physical symptoms in a cycle of depres-
sion and inflammation. This study’s aims to examine the mediator
roles of chronic illness-related shame and experiential avoidance
in the relationship between IBD symptomatology and depression,
while controlling for associated medical complications. The sam-
ple comprised 161 adult IBD patients (52 males and 109 females),
with a mean age of 36.73 (SD = 10.93), that completed validated
measures. The hypothesised model was tested through path analy-
ses. Results (see
Fig. 1 )showed that although IBD symptomatology
presented a direct effect of .13 on depression, the majority of its
impact was mediated through chronic illness-related shame and
experiential avoidance with an indirect effect of 0.22. Indeed, IBD
symptomatology seemed to lead to higher chronic illness-related
shame, which presented a direct effect on depression of .15 and
an indirect effect mediated by experiential avoidance of 0.37. This
model presented excellent goodness-of-fit indices. These findings
suggest that targeting shame and experiential avoidance in IBD
patients would have beneficial outcomes for patients’ well-being.
It thus seems that compassion and acceptance-based psychother-
apies should be included in treatment programs for IBD.
Fig. 1
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.297

















