
S246
24th European Congress of Psychiatry / European Psychiatry 33S (2016) S116–S348
Objective
This study explored the relationships between FAM
components and their effects on QoL in a Chinese sample.
Methods
A total of 401 Chinese patients with chronic muscu-
loskeletal pain completedmeasures of three core FAM components
(pain catastrophizing, pain-related fear, and pain anxiety) and QoL.
Cross-sectional structural equation modeling (SEM) assessed the
goodness of fit of the FAM for two QoL outcomes, Physical (Model
1) and Mental (Model 2). In both models, pain catastrophizing was
hypothesized to underpin pain-related fear, thereby influencing
pain anxiety and subsequently QoL outcomes.
Results
Results of SEM evidenced adequate data-model fit
(CFI
3
0.90) for the two models tested (Model 1: CFI = 0.93; Model 2:
CFI = 0.94). Specifically, pain catastrophizing significantly predicted
pain-related fear (Model 1: stdb = 0.90; Model 2: stdb = 0.91), which
in turn significantly predicted pain anxiety (Model 1: stdb = 0.92;
Model 2: stdb = 0.929) and QoL outcomes in a negative direction
(Model 1: stdb =
−
0.391; Model 2: stdb =
−
0.651) (all
P
< 0.001)
( Table 1 , F ig. 1 ).Conclusion
Our data substantiated the existing FAM literature
and offered evidence for the cross-cultural validity of the FAM in
the Chinese population with chronic pain.
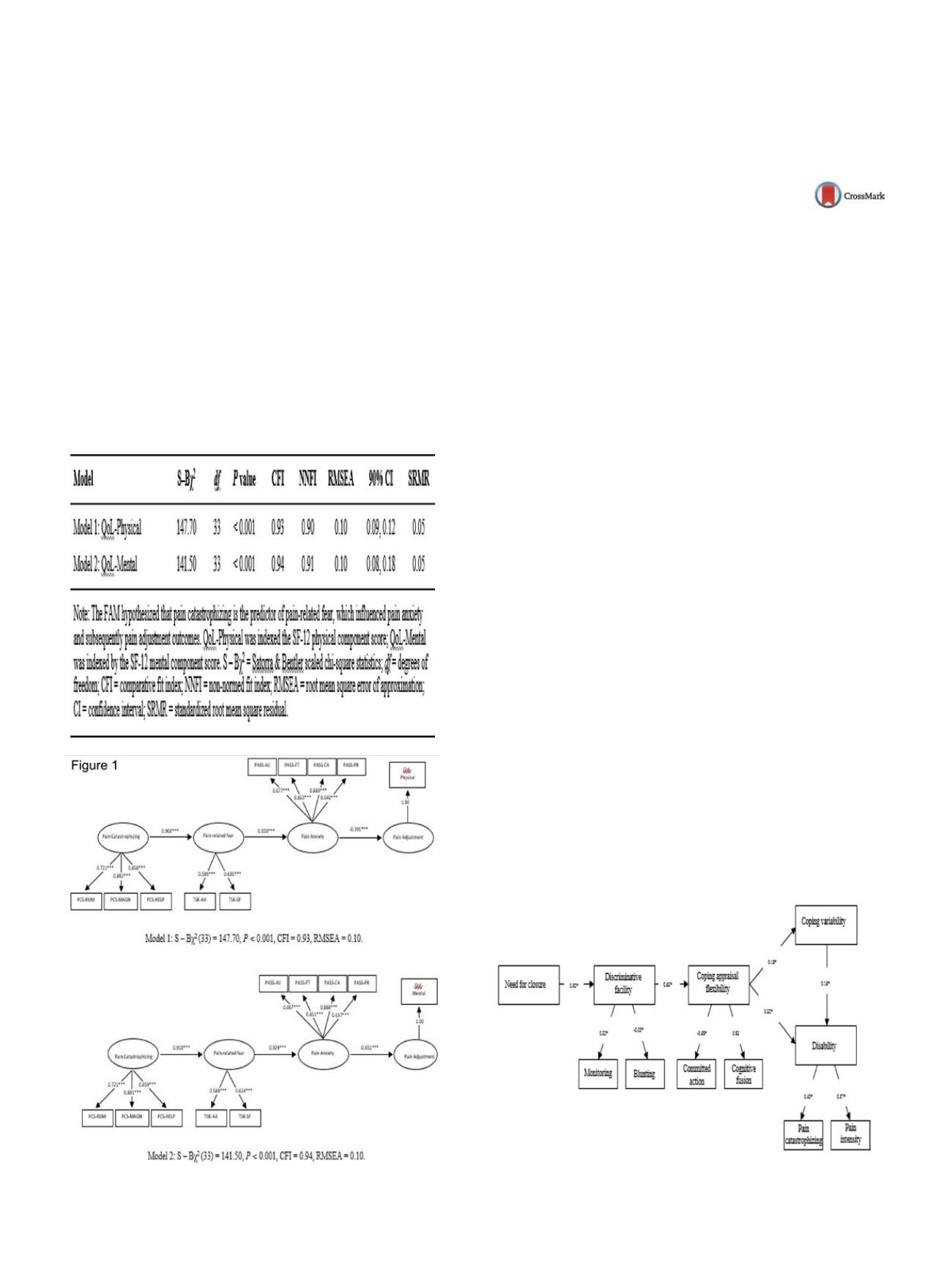
Table 1
Results of SEM testing the FAM for two QoL outcomes.
Fig. 1
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.497EW380
The role of coping flexibility in chronic
pain adjustment: Preliminary analysis
W. Wong
1 ,∗
, Y . Chow
2 , S. Wong
2 , P. Chen
3 , H.Lim
4 ,L. McCracken
5 , R.Fielding
61
Hong Kong Institute of Education, Dept of Special Education &
Counseling, Hong Kong, China
2
Queen Mary Hospital, Dept of Anesthesiology & Operating Services,
Hong Kong, China
3
Alice Ho Miu Ling Hospital, Dept of Anesthesiology & Operating
Services, Hong Kong, China
4
United Christian Hospital, Dept of Anesthesiology & Operating
Services, Hong Kong, China
5
King’s College London, Health Psychology Section, London, United
Kingdom
6
University of Hong Kong, School of Public Health, Hong Kong, China
∗
Corresponding author.
Introduction
While a body of research has evidenced the role of
pain coping in chronic pain adjustment, the role of coping flexibil-
ity in chronic pain adjustment has received little research attention.
Coping flexibility can be conceptualized with two dimensions, cog-
nitive and behavioral. The cognitive dimension of coping flexibility
(or coping appraisal flexibility) refers to one’s appraisal of pain
experience when changing coping strategies whereas the behav-
ioral dimension of coping flexibility denotes the variety of coping
responses individuals use in dealing with stressful demands.
Objective
The aim of this paper is to present preliminary find-
ings on the role of coping flexibility in chronic pain adjustment
by assessing 3 competing models of pain coping flexibility (see
Figs. 1–3 ).Methods
Patients with chronic pain (
n
= 300) completed a battery
of questionnaire assessing pain disability, discriminative facility,
need for closure, pain coping behavior, coping flexibility, and pain
catastrophizing. The 3 hypothesized models were tested using
structural equation modeling (SEM). In all models tested, need for
closure and discriminative facility were fitted as the dispositional
cognitive andmotivational factors respectively underlying the cop-
ing mechanism, whereas pain catastrophizing and pain intensity
were included as covariates.
Results
Results of SEM showed that the hierarchical model
obtained the best data-model fit (CFI = 0.96) whereas the other two
models did not attain an accept fit (CFI ranging from 0.70–0.72).
Conclusion
Our results lend tentative support for the hierarchical
model of pain coping flexibility that coping variabilitymediated the
effects of coping appraisal flexibility on disability.
Fig. 1
The hierarchical model (S-B
2
= 40.61, df = 24, CFI = 0.959,
NNFI = 0.94, EMSEA = 0.06, 90% CI = 0.02, 0.09).


















