
24th European Congress of Psychiatry / European Psychiatry 33S (2016) S349–S805
S559
EV655
Most common diagnoses in first
consultations on mental health
centers
C. Manso Bazús
∗
, J. Valdes Valdazo , E. Garcia Fernandez ,
L.T. Velilla Diez , J. Min Kim , C. Martinez Martinez ,
M.Á. Heredero Sanz
Complejo Asistencial Universitario de León, Psiquiatria, León, Spain
∗
Corresponding author.
Introduction
It often happens that primary care teams sends to
specialized care any type of demand without discriminating on
many times.
Objective
Study of diagnoses that get to the consultations.
Methodology
Retrospective observational study with data gath-
ered during 3 months of diagnosis carried out in the first
consultations.
Results
The study guides that there is much minor pathology in
the first consultation.
Conclusions
Currently, attention on mental health is over-
crowded because there is an excess of derivation from minor
pathologies. So, an adequate coordination and communicationwith
primary care could improve patients’ care.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.1640EV656
Analysis of demand in the first visit to
the mental health unit
B. Mata Saenz
∗
, E. Lopez Lavela , T. Rodríguez Cano ,
L. Beato Fernández
Hospital General Ciudad Real, Psychiatry, Ciudad Real, Spain
∗
Corresponding author.
Introduction
The first visit is crucial, since it is where a treatment
plan is selected and the decision to refer or not the patient to a
specialized unit is made. Mental care could be improved through
the centralization of demand and the identification of patients’ and
psychiatrists’ expectations.
Objectives
Analyzing patients’ and psychiatrists’ demands and
expectations in the first visit to use them as a starting point for
the planning and coordination of treatment actions.
Aims
To design a record system of the Minimum Basic Data Set
of the Centralized Department of our Unit.
Methods
This is an epidemiological, observational, prospective
study of patients referred to our department. Following variables
were collected:
– referral origin;
– reason;
– demographic data;
– diagnosis impression;
– destination of referral.
The Statistical Package for Social Science version 19.0 was used to
analyze the data.
Results
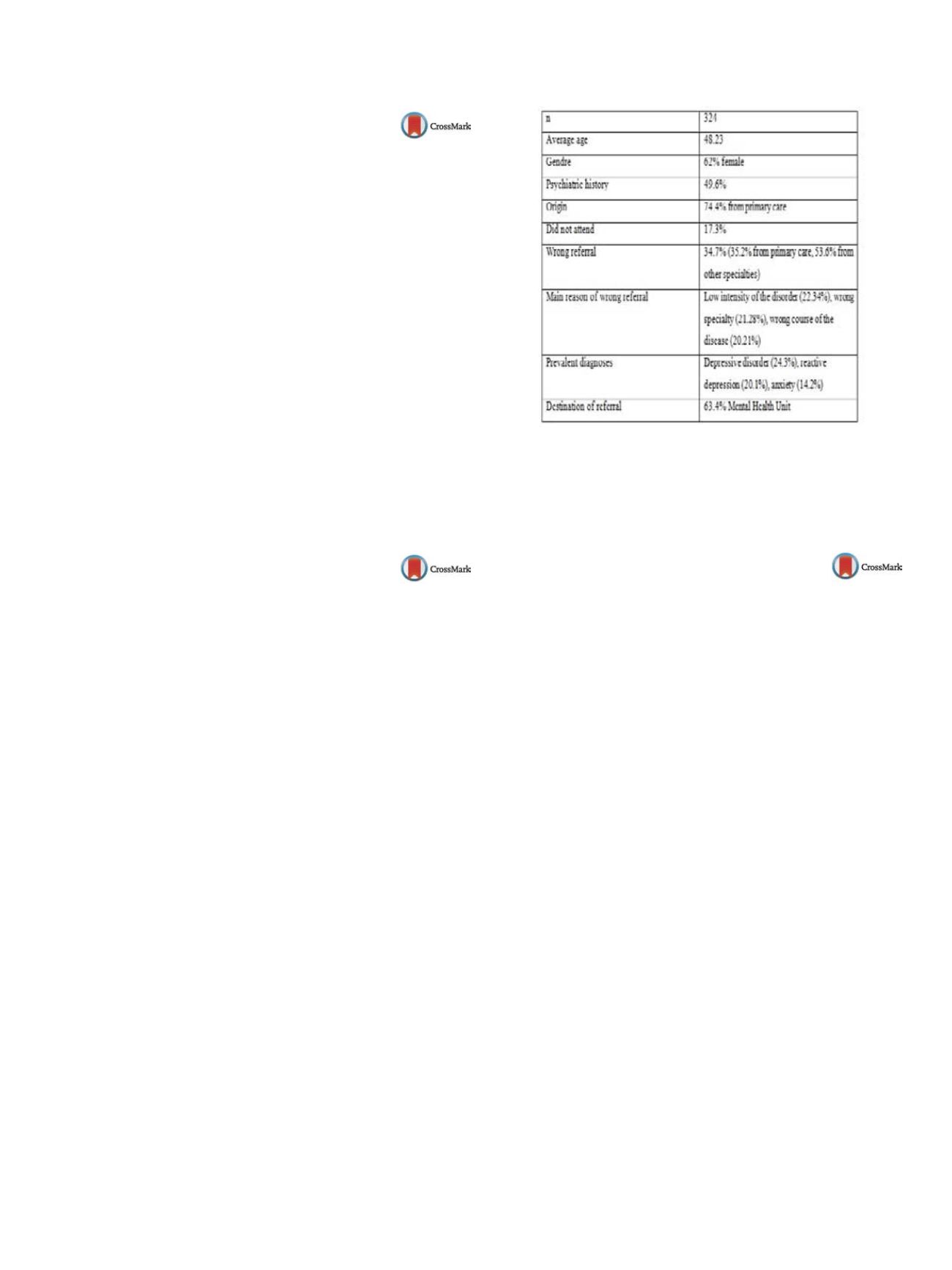
Table 1 .Conclusions
The data obtained are consistent with those reported
in the literature for this population. The high rate of wrong referrals
reveals the necessity of improving coordination and establishing
specific referral criteria. Some initiatives have been designed and
will be prospectively evaluated in the future.
Table 1
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.1641EV657
An evaluation of psychological
distress and social support of
survivors and contacts of Ebola virus
disease infection and their relatives in
Lagos, Nigeria – 2014
A. Mohammed
1 ,∗
, T. Sheikh
1, S. Gidado (Field coordinator)
2,
P. Nguku (Resident Advisor)
2, A. Olayinka (Resident Advisor)
2,
C. Ohuabunwo (Resident Advisor)
2,
W. Ndadilnasiya (Field coordinator)
2, A. Joseph
31
Federal Neuropsychiatric hospital, Clinical services, Kaduna, Nigeria
2
Nigerian Field Epidemiology and Laboratory Training Program,
Abuja, Nigeria
3
University of Lagos, Department of Psychiatry, Lagos, Nigeria
∗
Corresponding author.
Background
By September 2014, an outbreak of Ebola viral dis-
ease (EVD) in West African countries had recorded over 2200
deaths. EVD, create fear and panic among patients, and other stake-
holders, a risk factor for psychological distress, which could have
public health implication for control of EVD. We determined fac-
tors associated with psychological distress among survivors and
contacts of EVD and their relatives.
Methods
In a descriptive cross-sectional study, General Health
Questionnaire was used to assess psychological distress and Oslo
Social Support Scale was used to assess social support factors
associated with psychological distress were determined using
Chi
2
/odds ratio and adjusted odds ratio.
Results
Of the 117 participants, 78 (66.7%) were females. Most
frequently occurring psychological distress were inability to con-
centrate (37.6%) and loss of sleep over worry (33.3%). Losing a
relation to EVD outbreak (OR = 6.0, 95% CI: 1.2–32.9) was signifi-
cantly associated with feeling unhappy or depressed while being a
health worker was protective (OR = 0.4, 95% CI: 0.2–0.9). Adjusted
odds ratio (AOR) showed losing a relationwas a predictor of “feeling
unhappy or depressed” (AOR = 5.7, 95% CI: 1.2–28.0) and inability to
concentrate (AOR = 10.1, 95% CI: 1.7–60.7) while having no tertiary
education remained protective (AOR = 0.2, 95% CI: 0.1–0.6).
Conclusions
Survivors and contacts of EVD and their relations
develop psychological distress. Development of psychological dis-
tress was predicted by loss of family member. We recommended


















