
24th European Congress of Psychiatry / European Psychiatry 33S (2016) S349–S805
S665
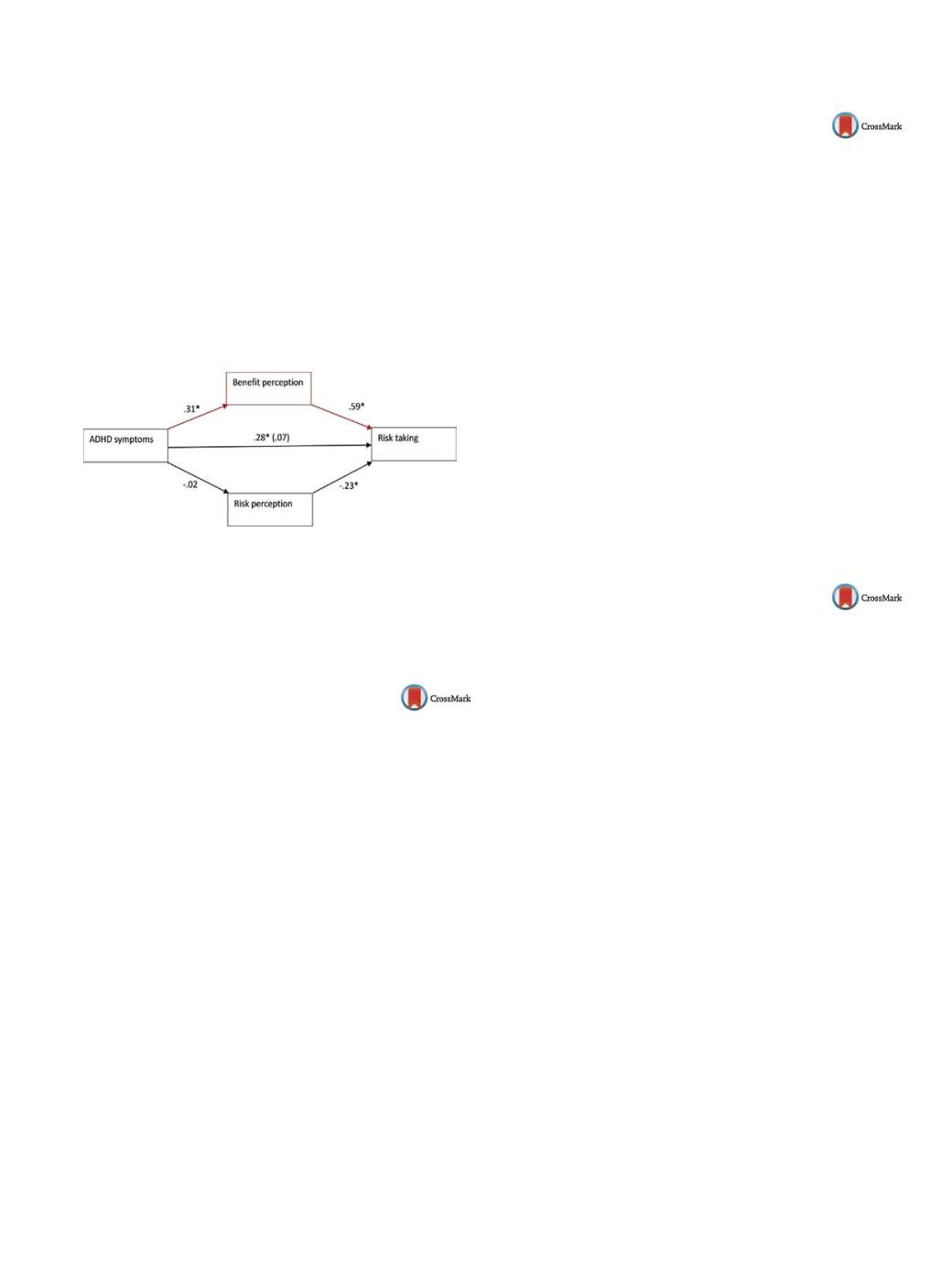
Attention deficit and hyperactivity disorder (ADHD) is associated
with increased engagement in risk-taking behaviors. The present
study aimed to further our knowledge regarding the extent and
the reasons for the association between ADHD symptoms and
risk-taking, using a theory-driven behavioral economy theory. The
Domain Specific Risk-Taking scale was used, on which 244 adults
rated the likelihood of engagement in a range of risky behaviors,
across five real life domains, as well as the magnitude of perceived
benefit and risk they ascribed to these behaviors. Level of ADHD
symptoms was positively correlated with engagement in risky
behaviors and benefit perception, but not with risk perception.
Mediation analysis confirmed that benefit perception, but not risk
perception, mediated the association between ADHD symptoms
and engagement in risk-taking behaviors
( Fig. 1 ).These findings
emphasize the role of benefit perception in facilitating risk-taking
by people with ADHD symptoms.
Fig. 1
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.1973EV989
The delusion of aurora (a structural
and dynamic analysis)
D. Porta Pelay
o 1 ,∗
, L . López Alonso
21
Hermanas Hospitalarias, Mental Health Area, Málaga, Spain
2
Psiquiatría, Psiquiatría, Las Palmas de Gran Canarias, Spain
∗
Corresponding author.
Introduction
The classical authors associate the insanity with
delusions, without delusions there was not insanity. This axiom
has changed nowadays, and it’s also accepted that insanity can exist
without delusions.
Aim
We aim to know and describe which factors are involved in
the development of the delusion. Use these conclusions to drive the
patient to the comprehension and acceptance of the reality.
Objective
(a) Unravel the mechanism of delusion, (b) seek the
causes, (c) find out an explanation about the origin and develop-
ment of the delusional thematic.
Method
Clinical biographic review, carried on in 2 steps: (a)
review the delusions store in the Hermanas Hospitalarias Spanish
hospitals (17 centres), (b) choose one of them, (c) use the induc-
tive method for analyzing the details and for making conclusions
in order to be apply in the delusional process.
Results
(a) Understand the internal dynamic of delusion and how
the delusion becomes the main axis of the patient life. (b) The
patient finds on the delusion a life motive, which did not exist
before.
Conclusion
Paraphrasing Dr.Castilla del Pino, “the delusion is a
necessary mistake”. From the emotional point of view, it can be
said “the delusion is a cry of a captured heart”.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.1974EV990
The psychopathology scan from the
phenomenology
S. Rodrígue Vargas
Almería, Spain
Introduction
This is a doctrinal movement that seeks to analyze
mental illness without reductionism and seeks to grasp the nearest
as possible to the reality of the patient.
Aims
This is the analysis of an event, a concept, a feeling, trying
to grasp as it is lived by the subject and in the direction you may
have for him.
Methods
Review of literature.
Results
It was the first approach to the knowledge of the patho-
logical experience and was the first scientific model to characterize
themental pathology. It was the central doctrine of psychiatry until
the end of World War II, when the hegemony of the German psy-
chiatric science gave way to the views that are primarily developed
in Anglo-Saxon countries (psychoanalysis and behavioral psychol-
ogy), although some European countries such as Germany and
Spain continued growing until the 1980s, when it culminated in
the publication of the DSM-III (1980).
Conclusions
These approaches are “old fashioned” but are essen-
tial to understand and know the reality of human sick, “mentally ill
man.”
Disclosure of interest
The author has not supplied his/her decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.1975EV991
Late paraphrenia. A case report
B. Serván Rendón-Luna
1 ,∗
, L. Reyes Molón
1,
R. Fernández García-Andrade
1, J. Fernández Aurrecoechea
21
Hospital Clínico San Carlos, Psychiatry, Madrid, Spain
2
Hospital Rey Juan Carlos, Psychiatry, Madrid, Spain
∗
Corresponding author.
Introduction
Paraphrenia is a chronic delusion, which may or
may not be accompanied by hallucinations, usually with a late
onset, and whose chronic course, unlike what it usually happens
in schizophrenia, is not typically associated to the schizophrenic
defect. When it appears in over 60-years-old people, we talk about
late paraphrenia.
Objective
Highlighting relevant aspects of paraphrenic symp-
toms and excluding entities such as dementia.
Methods
Bibliographical review in literature and pub med using
as keywords: “paraphrenia”; “megalomania”; “mystic-religious”;
“late psychosis”.
Results
We present the case of a 69-years-old woman who
showed megalomania, mystic-religious delusions, demonic pres-
ence and kinaesthetic and visual hallucinations. Brain SPECT: data
within normal limits, neuropsychological study: possible mild cog-
nitive impairment. First contact with psychiatry at age 63. History
of 3 psychiatric income with different diagnoses: “dissociative
state”, “acute polymorphic psychotic disorder” and “frontotem-
poral dementia”. The patient has been treated with different
treatments (lithium, neuroleptics and benzodiazepines). Along the
track has never been asymptomatic, presenting psychotic and
affective semiology.
Conclusions
A late paraphrenia case is shown. The study of senile
psychoses has been traditionally full of controversies. Entities such
as paraphrenia have been relegated in the current, however, it is a
disorder with differential characteristics within the psychotic spec-
trum, so it seems wrong to do without the diagnosis.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2016.01.1976

















